Mr Wijat's friend Magic Rabbit
Mr Wijat's friend Magic Rabbit  http://www.easterlingentertainment.net
http://www.easterlingentertainment.netINLNews YahooMail HotMail GMail AOLMai
lUSA MAIL YahooMail HotMailGMail AOLMail MyWayMail CNNWorld IsraelVideoNs
INLNsNYTimes WashNs AustStockEx WorldMedia JapanNs AusNs World VideoNs WorldFinance ChinaDaily IndiaNs USADaily BBC EuroNsABCAust
WANs NZNews QldNs MelbAge AdelaideNs TasNews ABCTas DarwinNsUSA MA
Stories Video/Audio Reuters AP AFP The Christian Science Monitor U.S. News & World Report AFP Features Reuters Life! NPR The Advocate Pew Daily Number Today in History Obituaries Corrections Politics LocalNews BBC News
USA WEEKLY NEWS EASY TO FIND HARD TO LEAVE
Visit International News Limited for the best values on:
domain names-domain transfers
INLNews YahooMail HotMail GMail AOLMail USA MAIL
HottestWebNews
Twitter //twitter.com/following
Comcast.net: News, Sports, Video, TV listings, Email and more!http://www.comcast.net/d/
www.facebook.com
Facebook is a social utility that connects people with friends and others who work, study and live around them. People use Facebook to keep up with friends,
//www.facebook.com/login.php
www.myspace.com/fringeshowshavetalent for entertaining fringe video clips
USA WEEKLY NEWS EASY TO FIND HARD TO LEAVE
Visit International News Limited for the best values on:
domain names-domain transfers
INLNews YahooMail HotMail GMail AOLMail USA MAIL
Click here to get you daily dose of Real Independent USA News with Amy Goodman at Domocracy Now
http://www.huffingtonpost.com/
GamingHarbor, Download Games to get 1000’s of Games!
http://www.gamingharbor.com/go.do?a=1805&l=4019
Welcome to Gaia | Gaia Onlinehttp://www.gaiaonline.com/
The Official Site of Major League Baseball: Events: 2009 All-Star Game Sprint Final Vote
http://mlb.mlb.com/mlb/events/all_star/y2009/fv/ballot.html
Make Money At Home Onlinehttp://www.howimadecash.com/a/
Read Free Manga Online at One Manga. Online manga scans reader.http://www.onemanga.com/
www.world-job-news.com http://www.world-job-news.com/finance/?t202id=89559&t202kw=lppop-1
Mozilla Firefox Start Page//www.google.com/firefox?client=firefox-a&rls=org.mozilla:en-US:o...
Inspirational Quote "The
beginning of love is to let those we love be perfectly themselves, and
not to twist them to fit our own image. Otherwise we love only the
reflection of ourselves we find in them.? Thomas Merton"
Click Here For Your Up To Date World Live Sports Scores
INLNews YahooMail HotMail GMail AOLMail USA MAILMyWayMail
CNNWorld IsraelVideoNs INLNsNYTimes WashNs WorldMedia JapanNs AusNs World VideoNs WorldFinance ChinaDaily IndiaNs USADaily BBC EuroNsABCAust
WANs NZNews QldNs MelbAge AdelaideNs
TasNews ABCTas DarwinNsUSA MAIL
ABC News Video FOX News Video FOXBusiness Video CNN Video AP Video BBC News Video Reuters Video AFP Video CNET Video
CNBC Video Australia 7 News Video Rocky Mountain News Elections Video CBC.ca Video NPR Audio
Kevin Sites in the Hot Zone Video
Richard Bangs Adventures Video Charlie Rose Video Expanded Books Video Assignment Earth Video
ROOFTOPCOMEDY.com Video
Guinness World Records Video weather.com Video AccuWeather Video You Witness News User Video
NPR Audio BY CATEGORY Top Stories Politics World Business Sports
Technology Health & Science Arts U.S.
VIEW LOCAL VIDEO KVUE-TV Austin WJZ 13 Baltimore WBZ Boston
WCNC Charlotte CBS 2 Chicago
CBS 11 Dallas CBS4 Denver 13 News, WVEC Hampton Roads 11 News Houston
CBS 2 / KCAL 9 Los Angeles
WHAS TV11 Louisville CBS4 Miami WCCO Minneapolis WWL-TV,
Channel 4 New Orleans CBS 2 New York
CBS 3 Philadelphia KTVK 3TV Phoenix KDKA Pittsburgh
KGW NewsChannel 8 Portland, Ore. WRAL.com Raleigh
CBS 13 / CW 31 Sacramento KENS 5 - TV San Antonio Channel 8 San Diego
CBS 5 San Francisco
KING5 Seattle KREM.com Spokane/Coeur d'Alene KMOV
Channel 4 St. Louis FOX 11 Tucson
Video by Category
U.S. Business World Entertainment Sports Tech Politics Science
Health Environment Weather Opinion Odd
Video by Topic Campaign '08 Wall Street Iraq Gas Prices Mideast Conflict
Climate Change
More INL News Video !Finance Sports
![]()
Hi there.welcome to YahooRealEstate.com.au Yahoo!!!!!!!Click here for the cheapest real estate advertising on the internet
 STUNTMAN: Jon Templeton will act as Hugh Jackman's stunt double in the film Australia. Picture: MEGAN RAYLE
STUNTMAN: Jon Templeton will act as Hugh Jackman's stunt double in the film Australia. Picture: MEGAN RAYLE
Click Here For Your Up To Date World Live Sports Scores
USAWeeklyNews.com
http://usaweeklynews.com/Home_Page.html
USADailyNews http://www.usatoday.com/
USNews.com http://www.usnews.com/ USWeekly.com http://www.usweekly.com/
USANews.net http://www.usanews.net/
More Great World News Links
World Liberal News Links
Conservative News
NEWS NBA NHL Tennis Golf NFL Soccer NASCAR WORLD LOCAL FINANCE
Web Directory Listings of the top sites in each category.
Blog Web Discovery Machine
- In Time for Summer, Top Travel Sites
Jun 30, 2009 Posted by Geoffrey Mack
- Facebook Juggernaut Overtakes YouTube
Jun 10, 2009 Posted by Geoffrey Mack
- Don't forget the Grads... Top Used Car Sites
More News LINKS
NEWS SOURCES
BLOGS
COLUMNISTS
ALL THINGS ARIANNA
More News LINKS
NEWS SOURCES
BLOGS
COLUMNISTS
ALL THINGS ARIANNA
Mon, 20 Oct 2008
http://www.diabetes.co.uk/news/2008/Oct/2.5-million-people-with-diabetes-in-the-uk.html
According to the latest figures from Diabetes UK, the diabetic population of the UK has soared by some 167,000 in the last year. The total, according to the report, now stands are just under 2.5 million.
In England alone, this 6.4 per cent increase has resulted in the population crossing the two million mark for the first time. The vast majority of people with diabetes in the UK have type 2, often associated with obesity . Estimates put the obesepopulation of the UK at around 5 million.
The chief executive of Diabetes UK, Douglas Smallwood, reportedly commented: "These are truly alarming figures. Part of why we have seen such a huge increase can be attributed to improved screening from healthcare services and greater awareness amongst those at high risk oftype 2 diabetes . However, there is no getting away from the fact that this large increase is linked to the obesity crisis ."
The answer to the problem, according to Smallwood, lies in raising awareness. He reportedly continued: "We need to do all we can to raise awareness of the seriousness of diabetes and help people understand how a healthy lifestyle can help reduce their risk of developing type 2 diabetes."
Search results from diabetes.co.uk
http://www.diabetes.co.uk/results.asp?q=diabetes+uk&client=google-csbe&cx=007373116414207289069:bexng2zwcby&cof=FORID:11
-
Diabetes Diagnosis
Diagnosis for both type 1 and type 2 diabetes can occur in a number of different ways.
www.diabetes.co.uk/Diabetes-diagnosis.html -
Diabetes Search Results for Diabetes Uk
Diabetes.co.uk. Web. Diabetes Products. Desang Kitbags · Medi-Tag Jewellery · Zsweet - Natural Sweetener · See all products. Share Us ...
www.diabetes.co.uk/results.asp?q=diabetes+UK&client=google-csbe&cx=007373116414207289069:bexng2zwcby&cof=FORID:11 -
Exercise for Diabetics
People with diabetes are encouraged to exercise regularly for better blood sugar control and to reduce the risk of cardiovascular diseases.
www.diabetes.co.uk/exercise-for-diabetics.html -
Diabetes & Diabetic News, Updated Daily
Diabetes news updated daily regarding all aspects of diabetes, including diabetes drugs, research, breakthroughs, illnesses, companies and other information ...
www.diabetes.co.uk/news/index.html -
People with diabetes not getting psychological support
Apr 8, 2009 ... According to the leading health charity Diabetes UK, as many as 85 per cent of adults suffering from diabetes in the UK are lacking access ...
www.diabetes.co.uk/news/2009/Apr/people-with-diabetes-not-getting-psychological-support.html -
Diabetes Forum • The Global Diabetes Community
This forum is the centre of the new community section of Diabetes.co.uk. Meet here to discuss diabetes issues, get help about diabetes, meet other diabetics ...
www.diabetes.co.uk/diabetes-forum/ -
DVLA facing petition about diabetes stance
Apr 30, 2009 ... The Driving and Vehicle Licensing Authority is facing a petition about its stance on diabetes . A petition has been issued calling for the ...
www.diabetes.co.uk/news/2009/Apr/dvla-facing-petition-about-diabetes-stance.html -
Diabetes UK Careline - Contact Careline Scotland
Diabetes UK, the leading UK diabetes charity, offers a unique service known as theDiabetes UK Careline. This is a service provided by Diabetes.org.uk, ...
www.diabetes.co.uk/diabetes-uk-careline.html -
Treatment for Diabetes
Successful treatment makes all the difference to long-term health, and achieving balanceddiabetes treatment can be the key to living with both type 1 and ...
www.diabetes.co.uk/treatment.html -
Blood Sugar Glucose Converter for Diabetes
Convert blood sugar/glucose from mmol/L (UK standard) to mg/dl (US standard) and vice versa using our blood sugar converter.
www.diabetes.co.uk/blood-sugar-converter.html -
About Us - Diabetes.co.uk
Diabetes.co.uk is part of the SFN Network of websites, based in the heart of England.Diabetes.co.uk has grown over the past 3 years into a vast diabetes ...
www.diabetes.co.uk/about.html -
Diabetes UK Charity
Diabetes UK is the UK's leading diabetes charity, celebrating its 75th anniversary this year. Founded in 1934, Diabetes UK has over 170000 members and works ...
www.diabetes.co.uk/diabetes-charity/diabetes-uk.html -
Diabetes Help & Support
Diabetes.co.uk is here to help and support diabetics and those affected by diabetes. This is a free, community-led information and support resource for ...
www.diabetes.co.uk/diabetes-help.html -
Contact Diabetes.co.uk
Contact the team at Diabetes.co.uk, based in Coventry, England.
www.diabetes.co.uk/contact.html -
Diabetes Test Strips
Blood glucose test strips (diabetes test strips) are one of the components of a diabetesmonitoring system. Diabetic test strips are an essential part of ...
www.diabetes.co.uk/diabetes_care/diabetes-test-strips.html -
Insulin in the UK
Insulin may be a key part of your treatment if you suffer from Diabetes. Insulin enables your body to use glucose. Different types of insulin can act very ...
www.diabetes.co.uk/insulin-in-the-uk.html -
Diabetes Charity Directory - Donate Online to UK & US Diabetes ...
Diabetes.co.uk aims to give its visitors the chance to learn more about individualdiabetes charities in the UK and US and what they do.
www.diabetes.co.uk/diabetes-charities.html -
Diabetes UK release new viral film
Sep 18, 2008 ... The Leading UK diabetes charity has taken a novel approach to spreading the message about type 1 diabetes . Available both online and via ...
www.diabetes.co.uk/news/2008/Sep/diabetes-uk-release-new-viral-film.html -
Diabetes Forum • Your chance to tell Diabetes UK what you want!
Diabetes UK produces information for young people like you about how to look after yourdiabetes and how to fit it into your daily life. ...
www.diabetes.co.uk/diabetes-forum/viewtopic.php?f=16&t=6884 -
UK Diabetes Industry
UK diabetes companies - A directory of major UK diabetes companies, diabetes business and pharmaceutical companies, the diabetes industry.
www.diabetes.co.uk/diabetes-industries.html -
Useful Links - Diabetes.co.uk
This section of diabetes.co.uk aims to provide a resource for diabetic patients who are interested in finding out more about their condition online.
www.diabetes.co.uk/links.html -
Diabetes UK in Second Life
Oct 24, 2008 ... The leading UK diabetes charity, Diabetes UK, have launched their new Silent Assassin campaign in Second Life. Second Life is a virtual ...
www.diabetes.co.uk/news/2008/Oct/diabetes-uk-in-second-life.html -
Diabetes UK launch new campaign
Leading UK diabetes charity, Diabetes UK, has launched a fresh new hard-hitting UK diabetes campaign. The advertising campaign, called Silent Assassin, ...
www.diabetes.co.uk/news/2008/Oct/Diabetes-UK-launch-new-campaign.html -
Glossary - A
ABPS, acronym for American Board of Podiatric Surgery Certification.
www.diabetes.co.uk/glossary/a.html -
New chairman for Diabetes UK
Diabetes news this morning carries reports that emergency care tsar of the government will take the helm of diabetes charity Diabetes UK .
www.diabetes.co.uk/news/2009/Feb/New-chairman-for-Diabetes-UK.html -
Diabetes And Stem Cell Research
Understanding the root causes of diabetes has eluded researchers for many years now. The way in which the immune system causes the destruction of precious ...
www.diabetes.co.uk/Diabetes-And-Stem-Cell-Research.html
Main / Side Dishes Desserts, Snacks and other Treats Soups and Salads Thanksgiving Recipes Enjoy these recipes that are not only delicious but Versatile Vegetable Corn Muffins You can use various vegetables to make these muffins both moist and lower in fat. Preheat oven to 400 degrees. Grease 12 cup muffin tin with non-stick cooking spray. Mix together dry ingredients in a medium bowl. Mix together wet ingredients in a small bowl. Add to the dry mixture and stir until just blended. Pour mixture into muffin tin, filling cups 3/4 full. Bake for 20 to 25 minutes. Per muffin:
DiabetesAction.org
http://www.diabetesaction.org/site/PageNavigator/Tips/tip
All diabetes questions are answered by Jane DeVane, MS, RD, CDE,
a Registered Dietician with a degree in exercise physiology and a certification in diabetes education. Her focus is an integrative approach to healing including management of diabetes, autoimmune and chronic conditions.
Heathly Recepies from DiabetesAction.org
also especially healthy for people with diabetes.
See bottom of this page for more copies of these healthy recipiesor click here http://www.diabetesaction.org/site/PageServer?pagename=recipe
Makes 12 muffins
Lentil Barley Stew A bowl of this stew satisfies hunger and helps stabilize blood sugar levels. It is also high in protein and water soluble fiber. Combine all ingredients in a large heavy stew pot. Cover and simmer for about 1 1/2 hours over low heat, stirring occasionally. Adjust seasonings to suit your taste. Makes 4 servings Mixed Vegetable Stir-Fry Heat sesame oil in wok or large skillet until hot. Add ginger root and garlic. Stir-fry about 1 minute or until light brown. Add broccoli, carrots and onion; stir-fry 1 minute. Stir in vegetable broth. Cover and cook about 3 minutes or until carrots are tender. Mix cornstarch and cold water; stir into vegetable mixture. Cook and stir about 10 seconds or until thickened. Add water chestnuts, mushrooms and oyster sauce. Cook and stir 30 seconds. Serve over brown rice or whole grain noodles if desired. Makes 4 servings Per serving (without rice or noodles): Roasted Pumpkin Seeds This crunchy snack is so easy and delicious there's no need to only make them at Halloween! Pumpkin seeds are a great source of magnesium, iron, zinc, essential fatty acids, and protein. They are also low in carbohydrate. Scrape seeds from the inside of a pumpkin. Rinse the pumpkin pulp off as well as you can and pat dry. Preheat oven to 150 degrees F (75 degrees C). Roasting on this lower heat helps to maintain more of the healthy essential fatty acids. Combine all ingredients in bowl; stir to coat all the seeds. Spread the seeds in a single layer on a baking sheet. Bake until seeds are golden brown (about 20 minutes), stirring occasionally. Adjust seasonings to suit your taste. Experiment: try adding a bit of brown sugar for sweet and salty seeds or paprika and celery salt for a spicy batch. Makes 4 servings Baked Spinach Ingredients: Directions: Melt butter in a large skillet over medium-high heat. Add onions and sauté until golden. Remove from heat. Stir in spinach, parmesan cheese, ricotta cheese, nutmeg, garlic powder, salt and pepper. Spoon into a 9-inch pie pan that has been sprayed with non-stick cooking spray. Combine tomato sauce, oregano and basil. Spread evenly over spinach mixture. Bake uncovered at 350 for 25 minutes. Let stand for 5 minutes before serving. Makes 4 servings
Per serving:
Per 1/4 cup serving:
Per serving:
Taiwanese Biotechnology Firm Introduces Possible Solution To Glucose Tolerance Lack Among Type II Diabetics Dr. Frank Mao Chia Hung of Maxluck Biotechnology Corporation explained contrary to common belief that diabetes is an ailment, it is more the inability of the glucose to enter the cells rather than the failure of the pancreas to produce insulin. Using biotechnology he invented an element called trivalent chromium, which helps the glucose enter the cell and be converted as energy, instead of remaining in the blood and causing high blood sugar among Type II diabetics. Trivalent chromium mimics the action of colostrum, found in mother's milk. Colostrum has large amounts of antibodies that protects the baby's vital body parts and plays a major role in producing chemical reactions to maintain life, including the conversion of glucose into energy. But since mother's milk is not available except for her newborn, Mao tapped biotechnology to come up with trivalent chromium. Initially, Maxluck manufactured it as milk powder, but because of complaints by some diabetics of lactose intolerance, the company produced a second generation of trivalent chromium in capsule form. Aside from helping Type II diabetics reduce their dependence on oral medication which often has side effects, trivalent chromium has been proven to help obese diabetics deal with their weight problems. The GTF products are expected to be accepted widely by Filipinos, many of whom are prone to diabetes because of genetic predisposition and the Filipino diet that is high in sugar and fat contents. Worldwide, there are 250 million diabetics, expected to double within the next 30 years, Mao said. RELATED HEALTH INFORMATION
http://www.vitabeat.com/taiwanese-biotechnology-firm-introduces-possible-solution-to-glucose-tolerance-lack-among-type-ii-diabetics/v/7710/
A Taiwanese biotechnology company is bringing into the Philippines a possible solution for the glucose tolerance factor lack among Type II diabetics. Tainan-based Maxluck Biotechnology is launching on Thursday the GT and F milk, which helps human cells absorb glucose.
Diabetes effects millions of people in the world and is an important subject to keep in public discussions and blogs...and is the subject of new research involving potential treatment of diabetes that could help millions of people live a more fullfulling life.. Diabetes mellitus (, often referred to simply as diabetes compass, dividers stemming from the verb "to pass through", consisting of the prefix da dia across, through and the verb to go, to walk) , is a syndrome of disordered metabolism, usually due to a combination of hereditary and environmental causes, resulting in abnormally high blood sugar levels (hyperglycemia).[2] Diabetes affects aproximately 18,000,000 children and adults in the United States, and perhaps 420,000,000 persons worldwide. Many millions of persons have diabetes but have not yet been diagnosed. Blood glucose levels are controlled by a complex interaction of multiple chemicals and hormones in the body, including the hormone insulin made in the beta cells of the pancreas. Diabetes mellitus refers to the group of diseases that lead to high blood glucose levels due to defects in either insulin secretion or insulin action in the body.[3] Diabetes develops due to a diminished production of insulin (in type 1) or resistance to its effects (in type 2 and gestational).[4] Both lead to hyperglycemia, which largely causes the acute signs of diabetes: excessive urine production, resulting compensatory thirst and increased fluid intake, blurred vision, unexplained weight loss, lethargy, and changes in energy metabolism. All forms of diabetes have been treatable since insulin became medically available in 1921, but there is no cure. The injections by asyringe, insulin pump, or insulin pen deliver insulin, which is a basic treatment of type 1 diabetes. Type 2 is managed with a combination of dietary treatment, exercise, medications and insulin supplementation. Diabetes and its treatments can cause many complications. Acute complications including hypoglycemia, ketoacidosis, ornonketotic hyperosmolar coma may occur if the disease is not adequately controlled. Serious long-term complications includecardiovascular disease, chronic renal failure, retinal damage, which can lead to blindness, several types of nerve damage, and microvascular damage, which may cause erectile dysfunction and poor wound healing. Poor healing of wounds, particularly of the feet, can lead to gangrene, and possibly to amputation. Adequate treatment of diabetes, as well as increased emphasis on blood pressure control and lifestyle factors such as not smoking and maintaining a healthy body weight, may improve the risk profile of most of the chronic complications. In the developed world, diabetes is the most significant cause of adult blindness in the non-elderly and the leading cause of non-traumatic amputation in adults, and diabetic nephropathy is the main illness requiring renal dialysis in the United States.[5] Classification The term diabetes, without qualification, usually refers to diabetes mellitus, which is associated with excessive sweet urine (known as "glycosuria") but there are several rarer conditions also named diabetes. The most common of these is diabetes insipidus in which the urine is not sweet (insipidus meaning "without taste" in Latin); it can be caused by either kidney (nephrogenic DI) or pituitary gland (central DI) damage. It is a noninfectious disease. Among the body systems affected are the nerve, digestive, circulatory, endocrine and urinary systems. The World Health Organization projects that the number of diabetics will exceed 350 million by 2030. Governments and other healthcare providers around the world are investing in health education, diagnosis and treatments for this chronic, debilitating - but controllable - disorder The term "type 1 diabetes" has universally replaced several former terms, including childhood-onset diabetes, juvenile diabetes, and insulin-dependent diabetes mellitus (IDDM). Likewise, the term "type 2 diabetes" has replaced several former terms, including adult-onset diabetes, obesity-related diabetes, and non-insulin-dependent diabetes mellitus (NIDDM). Beyond these two types, there is no agreed-upon standard nomenclature. Various sources have defined "type 3 diabetes" as, among others, gestational diabetes,[6] insulin-resistant type 1 diabetes (or "double diabetes"), type 2 diabetes which has progressed to require injected insulin, and latent autoimmune diabetes of adults (or LADA or "type 1.5" diabetes.[7]) There is also maturity onset diabetes of the young (MODY) which is a group of several single gene (monogenic) disorders with strong family histories that present as type 2 diabetes before 30 years of age. Type 1 diabetes Diabetes mellitus type 1 (type I diabetes, T1D, T1DM, IDDM, juvenile diabetes) is a form of diabetes mellitus. Type 1 diabetes is anautoimmune disease [1] that results in destruction of insulin-producing beta cells of the pancreas. Lack of insulin causes an increase of fasting blood glucose (around 70-120 mg/dL in nondiabetic people) that begins to appear in the urine above the renal threshold (about 190-200 mg/dl in most people), thus connecting to the symptom by which the disease was identified in antiquity, sweet urine. Glycosuria or glucose in the urine causes the patients to urinate more frequently, and drink more than normal (polydipsia). Classically, these were the characteristic symptoms which prompted discovery of the disease. Type 1 is lethal unless treated with exogenous insulin. Injection is the traditional and still most common method for administering insulin; jet injection, indwelling catheters, and inhaled insulin has also been available at various times, and there are several experimental methods as well. All replace the missing hormone formerly produced by the now non-functional beta cells in the pancreas. In recent years, pancreas transplants have also been used to treat type 1 diabetes. Islet cell transplant is also being investigated and has been achieved in mice and rats, and in experimental trials in humans as well[2]. Use of stem cells to produce a new population of functioning beta cells seems to be a future possibility, but has yet to be demonstrated even in laboratories as of 2008. Type 1 diabetes (formerly known as "childhood", "juvenile" or "insulin-dependent" diabetes) is not exclusively a childhood problem; the adult incidence of type 1 is noteworthy — many adults who contract type 1 diabetes are misdiagnosed with type 2 due to confusion on this point. There is currently no clinically useful preventive measure against developing type 1 diabetes, though a vaccine has been proposed and anti-antibody approaches are also being investigated. Most people who develop type 1 were otherwise healthy and of a healthy weight on onset, but they can lose weight quickly and dangerously, if not promptly diagnosed. Although the cause of type 1 diabetes is still not fully understood, and diet and exercise may help, the immune system damage is characteristic of type 1. The most definite laboratory test to distinguish type 1 from type 2 diabetes is the C-peptide assay, which is a measure of endogenous insulin production since external insulin has not (to date) included C-peptide. The presence of anti-islet antibodies (to Glutamic Acid Decarboxylase, Insulinoma Associated Peptide-2 or insulin), or lack of insulin resistance, determined by a glucose tolerance test, would also be suggestive of type 1. Many type 2 diabetics continue to produce insulin internally, and all have some degree of insulin resistance. Testing for GAD 65 antibodies has been proposed as an improved test for differentiating between type 1 and type 2 diabetes as it appears that the immune system malfunction is connected with their presence The cause of type 1 diabetes is still not fully understood. Some theorize that type 1 diabetes is generally a virally triggered autoimmune response in which the immune system's attack on virus infected cells is also directed against the beta cells in the pancreas. The autoimmuneattack may be triggered by reaction to an infection, for example by one of the viruses of the Coxsackie virus family or German measles, although the evidence is inconclusive. In type 1, pancreatic beta cells in the Islets of Langerhans are destroyed or damaged sufficiently to effectively abolish endogenous insulin production. This etiology distinguishes type 1's origin from type 2. It should also be noted that the use of insulin in treating a patient does not mean that patient has type 1 diabetes; the type of diabetes a patient has is determined only by the cause -- fundamentally by whether the patient is insulin resistant (type 2) or insulin deficient without insulin resistance (type 1). This vulnerability is not shared by everyone, for not everyone infected by the suspected organisms develops type 1 diabetes. This has suggested presence of a genetic vulnerability[3] and there is indeed an observed inherited tendency to develop type 1. It has been traced to particular HLA genotypes, though the connection between them and the triggering of an auto-immune reaction is still poorly understood. Some researchers believe that the autoimmune response is influenced by antibodies against cow's milk proteins.[4] A large retrospective controlled study published in 2006 strongly suggests that infants who were never breastfed had a risk for developing type 1 diabetes twice that of infants who were breastfed for at least three months.[citation needed] The mechanism is not fully understood. No connection has been established between autoantibodies, antibodies to cow's milk proteins, and type 1 diabetes. A subtype of type 1 (identifiable by the presence of antibodies against beta cells) typically develops slowly and so is often confused with type 2. In addition, a small proportion of type 1 cases have the hereditary condition maturity onset diabetes of the young(MODY) which can also be confused with type 2. Vitamin D in doses of 2000 IU per day given during the first year of a child's life has been connected in one study in Northern Finland (where intrinsic production of Vitamin D is low due to low natural light levels) with an 80% reduction in the risk of getting type 1 diabetes later in life. The causal connection, if any, is obscure. Some suggest that deficiency of Vitamin D3 (one of several related chemicals with Vitamin D activity) may be an important pathogenic factor in type 1 diabetes independent of geographical latitude, and so of available sun intensity.[citation needed] Some chemicals and drugs preferentially destroy pancreatic cells. Vacor (N-3-pyridylmethyl-N'-p-nitrophenyl urea), a rodenticide introduced in the United States in 1976, selectively destroys pancreatic beta cells, resulting in type 1 diabetes after accidental or intentional ingestion. Vacor was withdrawn from the U.S. market in 1979, but is still used in some countries. Zanosar is the trade name for streptozotocin, an antibiotic and antineoplastic agent used in chemotherapy for pancreatic cancer; it also kills beta cells, resulting in loss of insulin production. Other pancreatic problems, including trauma, pancreatitis or tumors (either malignant or benign), can also lead to loss of insulin production. The exact cause(s) of type 1 diabetes are not yet fully understood, and research on those mentioned, and others, continues. In December 2006, researchers from Toronto Hospital for Sick Children published research that shows a link between type 1 diabetes and the immune and nervous system. Using mice, the researchers discovered that a control circuit exists between insulin-producing cells and their associated sensory (pain-related) nerves.[5] It's being suggested that faulty nerves in the pancreas could be a cause of type 1 diabetes
What Wikipedia has to say on Diabetes
diabetes in cats and dogs.
Pathophysiology
Type 1 Diabetes is a polygenic disease, meaning many different genes contribute to its expression. Depending on locus or combination of loci, it can be dominant, recessive, or somewhere in between. The strongest gene, IDDM1, is located in the MHC Class II region on chromosome 6, at staining region 6p21. This is believed to be responsible for the histocompatibility disorder characteristic of type 1: Insulin-producing pancreas cells (beta cells) display improper antigens to T Cells. This eventually leads to the production of antibodies that attack these beta cells. Weaker genes are also located on chromosomes 11 and 18.
Environmental factors can strongly influence expression of type 1. A study showed that for identical twins, when one twin had type 1 diabetes, the other twin only had type 1 30-50% of the time. Despite having the exact same genome, one twin had the disease, where the other did not; this shows that environmental factors, in addition to genetic factors, can influence disease prevalence. [6]
Type 1 Diabetes is a polygenic disease, meaning many different genes contribute to its expression. Depending on locus or combination of loci, it can be dominant, recessive, or somewhere in between. The strongest gene, IDDM1, is located in the MHC Class II region on chromosome 6, at staining region 6p21. This is believed to be responsible for the histocompatibility disorder characteristic of type 1: Insulin-producing pancreas cells (beta cells) display improper antigens to T Cells. This eventually leads to the production of antibodies that attack these beta cells. Weaker genes are also located on chromosomes 11 and 18.
Environmental factors can strongly influence expression of type 1. A study showed that for identical twins, when one twin had type 1 diabetes, the other twin only had type 1 30-50% of the time. Despite having the exact same genome, one twin had the disease, where the other did not; this shows that environmental factors, in addition to genetic factors, can influence disease prevalence. [6]
Treatment Type 1 is treated with insulin replacement therapy — usually by insulin injection or insulin pump, along with attention to dietary management, typically including carbohydrate tracking, and careful monitoring of blood glucose levels using Glucose meters. Today the most common insulins are produced using genetic recombination techniques; formerly, cattle or pig insulins were used, and even sometimes insulin from fish. Major suppliers include Eli Lilly and Company, Novo-Nordisk, and Sanofi-Aventis. A more recent trend, from several suppliers, is insulin analogs which are slightly modified insulins which have different onset of action times or duration of action times. Untreated type 1 diabetes commonly leads to coma, often from diabetic ketoacidosis, which is fatal if untreated. At present, insulin treatment must be continued for life; this may perhaps change if better treatment, or a cure, becomes clinically available. Continuous glucose monitors have been developed and marketed which can alert patients to the presence of dangerously high or low blood sugar levels, but the general lack of widespread insurance coverage (certainly in the US) and technical limitations has limited the impact these devices have had on clinical practice so far. In more extreme cases, a pancreas transplant can restore proper glucose regulation. However, the surgery and accompanying immunosuppression required is considered by many physicians to be more dangerous than continued insulin replacement therapy, and is therefore often used only as a last resort (such as when a kidney must also be transplanted, or in cases where the patient's blood glucose levels are extremely volatile). Experimental replacement of beta cells (by transplant or from stem cells) is being investigated in several research programs and may become clinically available in the future. Thus far, beta cell replacement has only been performed on patients over age 18, and with tantalizing successes amidst nearly universal failure. Pancreas transplants are generally performed together with or some time after a kidney transplant. One reason for this is that introducing a new kidney requires takingimmunosuppressive drugs anyway, and this allows the introduction of a new, functioning pancreas to a patient with diabetes without any additional immunosuppressive therapy. However, pancreas transplants alone can be wise in patients with extremely labile type 1 diabetes mellitus.[7] Islet cell transplantation is expected to be less invasive than a pancreas transplant which is currently the most commonly used approach in humans. In one variant of this procedure, islet cells are injected into the patient's liver, where they take up residence and begin to produce insulin. The liver is expected to be the most reasonable choice because it is more accessible than the pancreas, and islet cells seem to produce insulin well in that environment. The patient's body, however, will treat the new cells just as it would any other introduction of foreign tissue, unless a method is developed to produce them from the patient's own stem cells or there is an identical twin available who can donate stem cells. The immune system will attack the cells as it would a bacterial infection or a skin graft. Thus, patients now also need to undergo treatment involving immunosuppressants, which reduce immune system activity. Recent studies have shown that islet cell transplants have progressed to the point that 58% of the patients in one study were insulin independent one year after islet cell transplant.[8] Ideally, it would be best to use islet cells which will not provoke this immune reaction, but scientists in New Zealand are also looking into placing them within a protective housing derived of sea-weed which enables insulin to flow out and nutrients to flow in while protecting the islets from immune system attack via white blood cells. It is estimated that about 5%–10% of North American diabetes patients have type 1. The fraction of type 1 in other parts of the world differs; this is likely due to both differences in the rate of type 1 and differences in the rate of other types, most prominently type 2. Most of this difference is not currently understood. Variable criteria for categorizing diabetes types may play a part. Some notable people with type 1 are American football quarterback Jay Cutler, swimmer Gary Hall, Jr. and Nick Jonas. The Juvenile Diabetes Research Foundation (JDRF) is the major charitable organization in the USA and Canada devoted to type 1 diabetes research. JDRF's mission is to cure type 1 diabetes and its complications through the support of research. Since its founding in 1970, JDRF has contributed more than $1.3 billion to diabetes research, including more than $156 million in FY 2008. In FY 2008, the Foundation funded 1,000 centers, grants and fellowships in 22 countries. In November 2008 JDRF launched a new online social network for people with type 1 diabetes--*Juvenation. The International Diabetes Federation is a worldwide alliance of over 160 countries to address diabetes research and treatment. The American Diabetes Association funds some work on type 1 but devotes much of its resources to type 2 diabetes due to the increasing prevalence of the latter type. Diabetes Australia is involved in promoting research and education in Australia on both type 1 and type 2 diabetes. The Canadian Diabetes Association is also involved in educating, researching, and sustaining sufferers of type 1 Diabetics in Canada. Pacific Northwest Diabetes Research Institute conducts clinical and basic research on type 1 and type 2 diabetes. As of 2009, there is no known cure for diabetes mellitus type 1 in modern clinical use. Pancreas transplant is not practical (too few are available, and pancreas transplant is technically difficult. The requirement for immuno-suppressive drugs contributes to the unsatisfactory nature of pancreas transplant as a cure). Nor is a cure known from any other source including traditional or alternative medical practice. There is ongoing research on various approaches to curing diabetes type 1. Diabetes type 1 is caused by the destruction of enough beta cells to produce symptoms; these cells, which are found in the Islets of Langerhans in the pancreas, produce and secrete insulin, the single hormone responsible for allowing glucose to enter from the blood into cells (in addition to the hormone amylin, another hormone required for glucosehomeostasis). Hence, the phrase "curing diabetes type 1" means "causing a maintenance or restoration of the endogenous ability of the body to produce insulin in response to the level of blood glucose" and cooperative operation with counterregulatory hormones. This section deals only with approaches for curing the underlying condition of diabetes type 1, by enabling the body to endogenously, in vivo, produce insulin in response to the level of blood glucose. It does not cover other approaches, such as, for instance, closed-loop integrated glucometer/insulin pump products, which could potentially increase the quality-of-life for some who have diabetes type 1, and may by some be termed "artificial pancreas".
[edit]Pancreas transplantation
[edit]Islet cell transplantation
[edit]Prevalence
[edit]Research foundations
[edit]Cure
A biological approach to the artificial pancreas is to implant bioengineered tissue containing islet cells, which would secrete the amounts of insulin, amylin and glucagon needed in response to sensed glucose.
When islet cells have been transplanted via the Edmonton protocol, insulin production (and glycemic control) was restored, but at the expense of continued immunosuppression drugs. Encapsulation of the islet cells in a protective coating has been developed to block the immune response to transplanted cells, which relieves the burden of immunosuppression and benefits the longevity of the transplant.[9]
One concept of the bio-artificial pancreas uses encapsulated islet cells to build an islet sheet which can be surgically implanted to function as an artificial pancreas.[10]
This islet sheet design consists of:
- an inner mesh of fibers to provide strength for the islet sheet;
- islet cells, encapsulated to avoid triggering a proliferating immune response, adhered to the mesh fibers;
- a semi-permeable protective layer around the sheet, to allow the diffusion of nutrients and secreted hormones;
- a protective coating, to prevent a foreign body response resulting in a fibrotic reaction which walls off the sheet and causes failure of the islet cells.
Islet sheet with encapsulation research is pressing forward with large animal studies at the present, with plans for human clinical trials within a few years.
Clinical studies underway in New Zealand by Living Cell Technologies have encapsulated pig islet cells in a sea-weed derived capsule. This approach has had very positive clinical studies and is currently underway in human trials as of 2008. So far, treatment using this method of cell encapsulation has been proven safe and effective and is the first to achieve insulin independence in human trials without immunosupressant drugs.[11] Research undertaken at the Massachusetts General Hospital between 2001 and 2003 demonstrated a protocol to reverse type 1 diabetes in non-obese diabetic mice (a frequently used animal model for type 1 diabetes mellitus).[12] Three other institutions have had similar results, as published in the March 24, 2006 issue of Science. A fourth study by the National Institutes of Health achieved similar results, and also sheds light on the biological mechanisms involved.[13] Other researchers, most notably Dr. Aaron I. Vinik of the Strelitz Diabetes Research Institute of Eastern Virginia Medical School and a former colleague, Dr. Lawrence Rosenberg (now at McGill University) discovered in a protein they refer to as INGAP, which stands for Islet Neogenesis Associated Protein back in 1997. INGAP seems to be the product of a gene responsible for regenerating the islets that make insulin and other important hormones in the pancreas. INGAP has had commercialization difficulties. Although it has appeared promising, commercial rights have changed hands repeatedly, having once been owned by Procter & Gamble Pharmaceuticals, which eventually dropped it. Rights were then acquired by GMP Companies. More recently, Kinexum Metabolics, Inc. has since sublicensed INGAP from GMP for further clinical trials. Kinexum has continued development under Dr. G. Alexander Fleming, an experienced metabolic drug developer, who headed diabetes drug review at the FDA for over a decade. As of 2008, the protein had undergone Phase 2 Human Clinical Trials, and developers were analyzing the results. At the American Diabetes Association's 68th Annual Scientific Sessions in San Francisco, Kinexum announced a Phase 2 human clinical trial with a combination therapy, consisting of DiaKine's Lisofylline (LSF) and Kinexum's INGAP peptide, which is expected to begin in late 2008.[14] The trial will be unique in that patients who are beyond the 'newly diagnosed' period will be included in the study. Most current trials seeking to treat people with type 1 diabetes do not include those with established disease. Research is being done at several locations in which islet cells are developed from stem cells. In January 2006, a team of South Korean scientists has grown pancreatic beta cells, which can help treat diabetes, from stem cells taken from the umbilical cord blood of newborn babies. In April 2007, it was reported by the Times Online that 15 young Brazilian patients diagnosed with type 1 diabetes were able to naturally produce insulin once again after undergoing mild chemotherapy to temporarily weaken their immune systems and then injection of their own stem cells. This allowed the pancreatic beta cells to produce insulin. Since white blood cells were blocking the pancreas from producing insulin, Dr. Voltarelli and colleagues killed the immune cells, allowing the pancreas to secrete insulin once more.[15] However, there were no control subjects, which means that all of the processes could have been completely or partially natural. Secondly, no theory for the mechanism of cure has been promoted. It is too early to say whether the results will be positive or negative in the long run.[16] In September 2008, scientists from the University of North Carolina at Chapel Hill School of Medicine have announced their success in transforming cells from human skin into cells that produce insulin.[17] The skin cells were first transformed into stem cells and then had been differentiated into insulin-secreting cells.[18] However, other scientists have doubts, as the research papers fail to detail the new cells' glucose responsiveness and the amount of insulin they are capable of producing. Research undertaken at the Massachusetts General Hospital between 2001 and 2003 demonstrated a protocol to reverse type 1 diabetes in non-obese diabetic mice (a frequently used animal model for type 1 diabetes mellitus).[12] Three other institutions have had similar results, as published in the March 24, 2006 issue of Science. A fourth study by the National Institutes of Health achieved similar results, and also sheds light on the biological mechanisms involved.[13] Other researchers, most notably Dr. Aaron I. Vinik of the Strelitz Diabetes Research Institute of Eastern Virginia Medical School and a former colleague, Dr. Lawrence Rosenberg (now at McGill University) discovered in a protein they refer to as INGAP, which stands for Islet Neogenesis Associated Protein back in 1997. INGAP seems to be the product of a gene responsible for regenerating the islets that make insulin and other important hormones in the pancreas. INGAP has had commercialization difficulties. Although it has appeared promising, commercial rights have changed hands repeatedly, having once been owned by Procter & Gamble Pharmaceuticals, which eventually dropped it. Rights were then acquired by GMP Companies. More recently, Kinexum Metabolics, Inc. has since sublicensed INGAP from GMP for further clinical trials. Kinexum has continued development under Dr. G. Alexander Fleming, an experienced metabolic drug developer, who headed diabetes drug review at the FDA for over a decade. As of 2008, the protein had undergone Phase 2 Human Clinical Trials, and developers were analyzing the results. At the American Diabetes Association's 68th Annual Scientific Sessions in San Francisco, Kinexum announced a Phase 2 human clinical trial with a combination therapy, consisting of DiaKine's Lisofylline (LSF) and Kinexum's INGAP peptide, which is expected to begin in late 2008.[14] The trial will be unique in that patients who are beyond the 'newly diagnosed' period will be included in the study. Most current trials seeking to treat people with type 1 diabetes do not include those with established disease. Research is being done at several locations in which islet cells are developed from stem cells. In January 2006, a team of South Korean scientists has grown pancreatic beta cells, which can help treat diabetes, from stem cells taken from the umbilical cord blood of newborn babies. In April 2007, it was reported by the Times Online that 15 young Brazilian patients diagnosed with type 1 diabetes were able to naturally produce insulin once again after undergoing mild chemotherapy to temporarily weaken their immune systems and then injection of their own stem cells. This allowed the pancreatic beta cells to produce insulin. Since white blood cells were blocking the pancreas from producing insulin, Dr. Voltarelli and colleagues killed the immune cells, allowing the pancreas to secrete insulin once more.[15] However, there were no control subjects, which means that all of the processes could have been completely or partially natural. Secondly, no theory for the mechanism of cure has been promoted. It is too early to say whether the results will be positive or negative in the long run.[16] In September 2008, scientists from the University of North Carolina at Chapel Hill School of Medicine have announced their success in transforming cells from human skin into cells that produce insulin.[17] The skin cells were first transformed into stem cells and then had been differentiated into insulin-secreting cells.[18] However, other scientists have doubts, as the research papers fail to detail the new cells' glucose responsiveness and the amount of insulin they are capable of producing.
Islet cell regeneration approach
Stem cells approach
South Korea
Brazil
University of North Carolina
Islet cell regeneration approach
Stem cells approach
South Korea
Brazil
University of North Carolina
Gene Therapy Approach
Technology for gene therapy is advancing rapidly such that there are multiple pathways possible to support endocrine function, with potential to practically cure diabetes.[19]
- Gene therapy can be used to manufacture insulin directly: an oral medication, consisting of viral vectors containing the insulin sequence, is digested and delivers its genes to the upper intestines. Those intestinal cells will then behave like any viral infected cell, and will reproduce the insulin protein. The virus can be controlled to infect only the cells which respond to the presence of glucose, such that insulin is produced only in the presence of high glucose levels. Due to the limited numbers of vectors delivered, very few intestinal cells would actually be impacted and would die off naturally in a few days. Therefore by varying the amount of oral medication used, the amount of insulin created by gene therapy can be increased or decreased as needed. As the insulin producing intestinal cells die off, they are boosted by additional oral medications.[20]
- Gene therapy might eventually be used to cure the cause of beta cell destruction, thereby curing the new diabetes patient before the beta cell destruction is complete and irreversible.[21]
- Gene therapy can be used to turn duodenum cells and duodenum adult stem cells into beta cells which produce insulin and amylin naturally. By delivering beta cell DNA to the intestine cells in the duodenum, a few intestine cells will turn into beta cells, and subsequently adult stem cells will develop into beta cells. This makes the supply of beta cells in the duodenum self replenishing, and the beta cells will produce insulin in proportional response to carbohydrates consumed.[22]
Yonsei University
Scientists in the South Korean university of Yonsei have, in 2000, succeeded in reversing diabetes in mice and rats. Using a viral vector, a DNA encoding the production of an insulin analog was injected to the animals, which remained non-diabetic for at least the eight months duration of the study.[23]
Prevention
"Immunization" approach
If a biochemical mechanism can be found that prevents the immune system from attacking beta cells, it may be administered to prevent commencement of diabetes type 1. Several groups are trying to achieve this by causing the activation state of the immune system to change from Th1 state (“attack” by killer T Cells) to Th2 state (development of new antibodies). This Th1-Th2 shift occurs via a change in the type of cytokine signaling molecules being released by regulatory T-cells. Instead of pro-inflammatory cytokines, the regulatory T-cells begin to release cytokines that inhibit inflammation.[24] This phenomenon is commonly known as "acquired immune tolerance".
DiaPep277
A substance designed to cause lymphocyte cells to cease attacking beta cells, DiaPep277 is a peptide fragment of a larger protein called HSP60. Given as a subcutaneous injection, its mechanism of action involves a Th1-Th2 shift. Clinical success has been demonstrated in prolonging the "honeymoon" period for people who already have type 1 diabetes.[25] The product is currently being tested in people with latent autoimmune diabetes of adults (LADA). Ownership of the drug has changed hands several times over the last decade. In 2007, Clal Biotechnology Industries (CBI) Ltd., an Israeli investment group in the field of life sciences, announced that Andromeda Biotech Ltd., a wholly owned subsidiary of CBI, signed a Term Sheet with Teva Pharmaceutical Industries Ltd. to develop and commercialize DiaPep277.[26]
Intra-nasal insulin
There is pre-clinical evidence that a Th1-Th2 shift can be induced by administration of insulin directly onto the immune tissue in the nasal cavity. This observation has led to a clinical trial, called INIT II, which began in late 2006, based in Australia and New Zealand.
BCG research
Tumor necrosis factor-alpha, or TNF-a, is part of the immune system. It helps the immune system distinguish self from non-self tissue. People with type 1 diabetes are deficient in this substance. Dr. Denise Faustman theorizes that giving Bacillus Calmette-Guérin (BCG), an inexpensive generic drug, would have the same impact as injecting diabetic mice with Freund's Adjuvant, which stimulates TNF-a production. TNF-a kills the white blood cells responsible for destroying beta cells, and thus prevents, or reverses diabetes.[27] She has reversed diabetes in laboratory mice with this technique, but was only able to receive funding for subsequent research from The Iaccoca Foundation, founded by Lee Iacocca in honor of his late wife, who died from diabetes complications. Human trials are set to begin in 2008.
Diamyd
Diamyd is the name of a vaccine being developed by Diamyd Medical. Injections with GAD65, an autoantigen involved in type 1 diabetes, has in clinical trials delayed the destruction of beta cells for at least 30 months, without serious adverse effects. Patients treated with the substance showed higher levels of regulatory cytokines, thought to protect the beta cells.[28] Phase III trials are under way in the USA [29] and in Europe[30].[31][32] Two prevention studies, where the vaccine is given to persons who have not yet developed diabetes, will start in 2009[33][34].
Entities involved in research
This section is an incomplete list of mainly commercial companies but also other entities, namely governmental institutions and individual persons, actively involved in research towards finding a cure to diabetes type 1.
It does not list research funds, hospitals in which research is undertaken, etc., but only the industrious, actual developers of such products.
Entities are listed alphabetically along with their status of research in that field, so that also entities which ceased research into finding a cure to diabetes type 1 may be listed.
- Amylin Pharmaceuticals – is working toward finding a cure, and has a drug on the market called Symlin (pramlintide acetate) that helps in treating Type 1 diabetes
- Cerco Medical [1] – Present status: Unknown
- Denise Faustman [2] – Present status: Working on immune modification
- DeveloGen [3] – Present status: Developing DiaPep 277
- Diamyd Medical [4] – Present status: Developing GAD65-based vaccine (phase III trial started)
- Tolerx, Inc. [www.defendagainstdiabetes.com] - Present status: Now (4/2009) in Phase 3 clinical study of otelixizumab, an Fc-disabled, anti-CD3 monoclonal antibody in patients with new onset (diagnosis within last 10 weeks) type 1 diabetes.
See also
- Richard K. Bernstein (low-carb diabetes diet)
- The Kara Neumann case – "treatment" by prayers case resulting in death
Further reading
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) - Diabetes in America Textbook (PDFs)
References
- ^ ""Type 1 Diabetes Mellitus"". Retrieved on 2008-08-04.
- ^ ""One Step Closer to a Cure - Interview; Patrick Perry, Saturday Evening Post"". Retrieved on 2008-11-02.
- ^ "Donner", "Horst"; "Harald Rau, Paul G. Walfish, Jens Braun, Thorsten Siegmund, Reinhard Finke, Jürgen Herwig, Klaus H. Usadel and Klaus Badenhoop" ("2007"). ""CTLA4 Alanine-17 Confers Genetic Susceptibility to Graves’ Disease and to Type 1 Diabetes Mellitus"". "The Journal of Clinical Endocrinology & Metabolism Vol. 82, No. 1 143-146". "The Journal of Clinical Endocrinology & Metabolism". Retrieved on 2008-02-06.
- ^ content.nejm.org
- ^ "Canadian scientists reverse diabetes in mice". Retrieved on 2007-06-04.
- ^ http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=222100
- ^ Pancreas Transplantation: Indications and Consequences
- ^ "Islet cell transplant: Experimental treatment for type 1 diabetes - MayoClinic.com". Retrieved on 2007-06-04.
- ^ Cerco Medical: Science: Methods
- ^ Cerco Medical: Company: Islet Sheet Research
- ^ Living Cell Technologies web site: Diabecell
- ^ "November 13, 2003 Regeneration of insulin-producing islets may lead to diabetes cure". Retrieved on 2007-06-04.
- ^ Faustman DL, Tran SD, Kodama S, et al (2006). "Comment on papers by Chong et al., Nishio et al., and Suri et al. on diabetes reversal in NOD mice". Science 314 (5803): 1243; author reply 1243.doi:. PMID 17124308.
- ^ DiaKine Therapeutics and Kinexum Metabolics to Develop Novel Combination Treatment to Type 1 Diabetes
- ^ http://www.timesonline.co.uk/tol/comment/leading_article/article1637235.ece
- ^ Voltarelli JC, Couri CE, Stracieri AB, et al (2007). "Autologous nonmyeloablative hematopoietic stem cell transplantation in newly diagnosed type 1 diabetes mellitus". JAMA 297 (14): 1568–76.doi:. PMID 17426276.
- ^ http://www.eurekalert.org/pub_releases/2008-09/uonc-ust091708.php
- ^ http://www.jbc.org/cgi/content/abstract/M806597200v1
- ^ Gene Therapy Approaches to Diabetes
- ^ Mary Ann Liebert, Inc. - Cookie absent
- ^ hopkinsbayview.org
- ^ Engene Inc
- ^ Gene Therapy for Diabetes: Scientific American
- ^ jci.org
- ^ interscience.wiley.com
- ^ medicalnewstoday.com
- ^ Shinichiro Ryu, Shohta Kodama, Kazuko Ryu, David A. Schoenfeld & Denise L. Faustman. 2001. Reversal of established autoimmune diabetes by restoration of endogenous ß cell function. J. Clin. Invest. 108(1): 63-72.
- ^ New England Journal of Medicine: GAD Treatment and Insulin Secretion in Recent-Onset Type 1 Diabetes
- ^ Diamyd US Phase III Trial
- ^ Diamyd European Phase III Trial
- ^ Further Evidence for Lasting Immunological Efficacy of Diamyd Diabets Vaccine
- ^ Diamyd Announces Completion of Type 1 Diabetes Vaccine Trial with Long Term Efficcacy Demonstrated at 30 Months
- ^ MSNBC News: Pioneering Diamyd(r) Study to Prevent Childhood Diabetes Approved
- ^ Diamyd press release: Diamyd approved for groundbreking study in Norway
External links
- Beta Cell Biology Consortium - Team science with the aim of developing a cell-based therapy for type 1 diabetes
- Summary of Current Research in Type-1 Diabetes Cures
- Diabetes Section of The Hormone Foundation
- Juvenation a social network for people with type 1 diabetes created by the Juvenile Diabetes Research Foundation
- Online Diabetes Support Team at the Juvenile Diabetes Research Foundation
- Children with Diabetes
- Young Diabetics
- Type 1 Diabetes TrialNet
- Type 1 Diabetes at the American Diabetes Association
- National Diabetes Information Clearinghouse
Type 2 diabetes mellitus is characterized differently and is due to insulin resistance or reduced insulin sensitivity, combined with relatively reduced insulin secretion which in some cases becomes absolute. The defective responsiveness of body tissues to insulin almost certainly involves the insulin receptor in cell membranes. However, the specific defects are not known. Diabetes mellitus due to a known specific defect are classified separately. Type 2 diabetes is the most common type.
In the early stage of type 2 diabetes, the predominant abnormality is reduced insulin sensitivity, characterized by elevated levels of insulin in the blood. At this stage hyperglycemia can be reversed by a variety of measures and medications that improve insulin sensitivity or reduce glucose production by the liver. As the disease progresses, the impairment of insulin secretion worsens, and therapeutic replacement of insulin often becomes necessary.
There are numerous theories as to the exact cause and mechanism in type 2 diabetes. Central obesity (fat concentrated around the waist in relation to abdominal organs, but not subcutaneous fat) is known to predispose individuals to insulin resistance. Abdominal fat is especially active hormonally, secreting a group of hormones called adipokines that may possibly impair glucose tolerance. Obesity is found in approximately 55% of patients diagnosed with type 2 diabetes.[11] Other factors include aging (about 20% of elderly patients in North America have diabetes) and family history (type 2 is much more common in those with close relatives who have had it). In the last decade, type 2 diabetes has increasingly begun to affect children and adolescents, probably in connection with the increased prevalence of childhood obesity seen in recent decades in some places.[12]Environmental exposures may contribute to recent increases in the rate of type 2 diabetes. A positive correlation has been found between the concentration in the urine ofbisphenol A, a constituent of polycarbonate plastic from some producers, and the incidence of type 2 diabetes.[13]
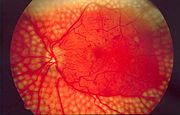
Type 2 diabetes may go unnoticed for years because visible symptoms are typically mild, non-existent or sporadic, and usually there are no ketoacidotic episodes. However, severe long-term complications can result from unnoticed type 2 diabetes, including renal failure due to diabetic nephropathy, vascular disease (including coronary artery disease), vision damage due to diabetic retinopathy, loss of sensation or pain due to diabetic neuropathy, liver damage from non-alcoholic steatohepatitis and heart failure fromdiabetic cardiomyopathy.
Type 2 diabetes is usually first treated by increasing physical activity, decreasing carbohydrate intake, and losing weight. These can restore insulin sensitivity even when the weight loss is modest, for example around 5 kg (10 to 15 lb), most especially when it is in abdominal fat deposits. It is sometimes possible to achieve long-term, satisfactory glucose control with these measures alone. However, the underlying tendency to insulin resistance is not lost, and so attention to diet, exercise, and weight loss must continue. The usual next step, if necessary, is treatment with oral antidiabetic drugs. Insulin production is initially only moderately impaired in type 2 diabetes, so oral medication (often used in various combinations) can be used to improve insulin production (e.g., sulfonylureas), to regulate inappropriate release of glucose by the liver and attenuate insulin resistance to some extent (e.g., metformin), and to substantially attenuate insulin resistance (e.g., thiazolidinediones). According to one study, overweight patients treated with metformin compared with diet alone, had relative risk reductions of 32% for any diabetes endpoint, 42% for diabetes related death and 36% for all cause mortality and stroke.[14]Oral medication may eventually fail due to further impairment of beta cell insulin secretion. At this point, insulin therapy is necessary to maintain normal or near normal glucose levels.
Gestational diabetes
Gestational diabetes mellitus (GDM) resembles type 2 diabetes in several respects, involving a combination of relatively inadequate insulin secretion and responsiveness. It occurs in about 2%–5% of all pregnancies and may improve or disappear after delivery. Gestational diabetes is fully treatable but requires careful medical supervision throughout the pregnancy. About 20%–50% of affected women develop type 2 diabetes later in life.
Even though it may be transient, untreated gestational diabetes can damage the health of the fetus or mother. Risks to the baby include macrosomia (high birth weight), congenital cardiac and central nervous system anomalies, and skeletal muscle malformations. Increased fetal insulin may inhibit fetal surfactant production and cause respiratory distress syndrome. Hyperbilirubinemia may result from red blood cell destruction. In severe cases, perinatal death may occur, most commonly as a result of poor placental perfusion due to vascular impairment. Induction may be indicated with decreased placental function. A cesarean section may be performed if there is marked fetal distress or an increased risk of injury associated with macrosomia, such as shoulder dystocia.
A 2008 study completed in the U.S. found that more American women are entering pregnancy with preexisting diabetes. In fact the rate of diabetes in expectant mothers has more than doubled in the past 6 years.[15] This is particularly problematic as diabetes raises the risk of complications during pregnancy, as well as increasing the potential that the children of diabetic mothers will also become diabetic in the future.
Other types
Most cases of diabetes mellitus fall into the two broad etiologic categories of type 1 or type 2 diabetes. However, many types of diabetes mellitus have known specific causes, and thus fall into separate categories as diabetes due to a specific cause. As more research is done into diabetes, many patients who were previously diagnosed as type 1 or type 2 diabetes will be reclassified as diabetes due to their known specific cause.
Some cases of diabetes are caused by the body's tissue receptors not responding to insulin (even when insulin levels are normal, which is what separates it from type 2 diabetes); this form is very uncommon. Genetic mutations (autosomal or mitochondrial) can lead to defects in beta cell function. Abnormal insulin action may also have been genetically determined in some cases. Any disease that causes extensive damage to the pancreas may lead to diabetes (for example, chronic pancreatitis and cystic fibrosis). Diseases associated with excessive secretion of insulin-antagonistic hormones can cause diabetes (which is typically resolved once the hormone excess is removed). Many drugs impair insulin secretion and some toxins damage pancreatic beta cells. The ICD-10 (1992) diagnostic entity, malnutrition-related diabetes mellitus (MRDM or MMDM, ICD-10 code E12), was deprecated by the World Health Organization when the current taxonomy was introduced in 1999.[4]
Signs and symptoms
The classical triad of diabetes symptoms is polyuria, polydipsia and polyphagia, which are, respectively, frequent urination, increased thirst and consequent increased fluid intake, and increased appetite. Symptoms may develop quite rapidly (weeks or months) in type 1 diabetes, particularly in children. However, in type 2 diabetes symptoms usually develop much more slowly and may be subtle or completely absent. Type 1 diabetes may also cause a rapid yet significant weight loss (despite normal or even increased eating) and irreducible mental fatigue. All of these symptoms except weight loss can also manifest in type 2 diabetes in patients whose diabetes is poorly controlled.
When the glucose concentration in the blood is raised beyond its renal threshold, reabsorption of glucose in the proximal renal tubuli is incomplete, and part of the glucose remains in the urine (glycosuria). This increases the osmotic pressure of the urine and inhibits reabsorption of water by the kidney, resulting in increased urine production (polyuria) and increased fluid loss. Lost blood volume will be replaced osmotically from water held in body cells and other body compartments, causing dehydration and increased thirst.
Prolonged high blood glucose causes glucose absorption, which leads to changes in the shape of the lenses of the eyes, resulting in vision changes; sustained sensible glucose control usually returns the lens to its original shape. Blurred vision is a common complaint leading to a diabetes diagnosis; type 1 should always be suspected in cases of rapid vision change, whereas with type 2 change is generally more gradual, but should still be suspected.
Patients (usually with type 1 diabetes) may also initially present with diabetic ketoacidosis (DKA), an extreme state of metabolic dysregulation characterized by the smell of acetone on the patient's breath; a rapid, deep breathing known asKussmaul breathing; polyuria; nausea; vomiting and abdominal pain; and any of many altered states of consciousness or arousal (such as hostility and mania or, equally, confusion and lethargy). In severe DKA, coma may follow, progressing to death. Diabetic ketoacidosis is a medical emergency and requires immediate hospitalization.
A rarer but equally severe possibility is hyperosmolar nonketotic state, which is more common in type 2 diabetes and is mainly the result of dehydration due to loss of body water. Often, the patient has been drinking extreme amounts of sugar-containing drinks, leading to a vicious circle in regard to the water loss.
[edit]Genetics
Both type 1 and type 2 diabetes are at least partly inherited. Type 1 diabetes appears to be triggered by some (mainly viral) infections, or less commonly, by stress or environmental exposure (such as exposure to certain chemicals or drugs). There is a genetic element in individual susceptibility to some of these triggers which has been traced to particular HLA genotypes (i.e., the genetic "self" identifiers relied upon by the immune system). However, even in those who have inherited the susceptibility, type 1 diabetes mellitus seems to require an environmental trigger. A small proportion of people with type 1 diabetes carry a mutated gene that causes maturity onset diabetes of the young(MODY).
There is a stronger inheritance pattern for type 2 diabetes. Those with first-degree relatives with type 2 have a much higher risk of developing type 2, increasing with the number of those relatives. Concordance among monozygotic twins is close to 100%, and about 25% of those with the disease have a family history of diabetes. Genes significantly associated with developing type 2 diabetes, include TCF7L2, PPARG, FTO, KCNJ11, NOTCH2, WFS1, CDKAL1, IGF2BP2, SLC30A8, JAZF1, and HHEX.[16] KCNJ11(potassium inwardly rectifying channel, subfamily J, member 11), encodes the islet ATP-sensitive potassium channel Kir6.2, and TCF7L2 (transcription factor 7–like 2) regulatesproglucagon gene expression and thus the production of glucagon-like peptide-1.[3] Moreover, obesity (which is an independent risk factor for type 2 diabetes) is strongly inherited.[17]
Monogenic forms, e.g. MODY, constitute 1-5 % of all cases.[18]
Various hereditary conditions may feature diabetes, for example myotonic dystrophy and Friedreich's ataxia. Wolfram's syndrome is an autosomal recessive neurodegenerative disorder that first becomes evident in childhood. It consists of diabetes insipidus, diabetes mellitus, optic atrophy, and deafness, hence the acronym DIDMOAD.[19]
Pathophysiology
Pathophysiology
Insulin is the principal hormone that regulates uptake of glucose from the blood into most cells (primarily muscle and fat cells, but not central nervous system cells). Therefore deficiency of insulin or the insensitivity of its receptors plays a central role in all forms of diabetes mellitus.
Most of the carbohydrates in food are converted within a few hours to the monosaccharide glucose, the principal carbohydrate found in blood and used by the body as fuel. The most significant exceptions arefructose, most disaccharides (except sucrose and in some people lactose), and all more complex polysaccharides, with the outstanding exception of starch. Insulin is released into the blood by beta cells (ß-cells), found in the Islets of Langerhans in the pancreas, in response to rising levels of blood glucose, typically after eating. Insulin is used by about two-thirds of the body's cells to absorb glucose from the blood for use as fuel, for conversion to other needed molecules, or for storage.
Insulin is also the principal control signal for conversion of glucose to glycogen for internal storage in liver and muscle cells. Lowered glucose levels result both in the reduced release of insulin from the beta cells and in the reverse conversion of glycogen to glucose when glucose levels fall. This is mainly controlled by the hormone glucagon which acts in an opposite manner to insulin. Glucose thus recovered by the liver re-enters the bloodstream; muscle cells lack the necessary export mechanism.
Higher insulin levels increase some anabolic ("building up") processes such as cell growth and duplication, protein synthesis, and fat storage. Insulin (or its lack) is the principal signal in converting many of the bidirectional processes of metabolism from a catabolic to an anabolic direction, and vice versa. In particular, a low insulin level is the trigger for entering or leaving ketosis (the fat burning metabolic phase).
If the amount of insulin available is insufficient, if cells respond poorly to the effects of insulin (insulin insensitivity or resistance), or if the insulin itself is defective, then glucose will not be absorbed properly by those body cells that require it nor will it be stored appropriately in the liver and muscles. The net effect is persistent high levels of blood glucose, poor protein synthesis, and other metabolic derangements, such as acidosis.
Diagnosis
The diagnosis of type 1 diabetes, and many cases of type 2, is usually prompted by recent-onset symptoms of excessive urination (polyuria) and excessive thirst (polydipsia), often accompanied by weight loss. These symptoms typically worsen over days to weeks; about a quarter of people with new type 1 diabetes have developed some degree of diabetic ketoacidosis by the time the diabetes is recognized. The diagnosis of other types of diabetes is usually made in other ways. These include ordinary health screening; detection of hyperglycemia during other medical investigations; and secondary symptoms such as vision changes or unexplainable fatigue. Diabetes is often detected when a person suffers a problem that is frequently caused by diabetes, such as a heart attack, stroke, neuropathy, poor wound healing or a foot ulcer, certain eye problems, certainfungal infections, or delivering a baby with macrosomia or hypoglycemia.
Diabetes mellitus is characterized by recurrent or persistent hyperglycemia, and is diagnosed by demonstrating any one of the following:[4]
- fasting plasma glucose level at or above 126 mg/dL (7.0 mmol/l).
- plasma glucose at or above 200 mg/dL (11.1 mmol/l) two hours after a 75 g oral glucose load as in a glucose tolerance test.
- symptoms of hyperglycemia and casual plasma glucose at or above 200 mg/dL (11.1 mmol/l).
A positive result, in the absence of unequivocal hyperglycemia, should be confirmed by a repeat of any of the above-listed methods on a different day. Most physicians prefer to measure a fasting glucose level because of the ease of measurement and the considerable time commitment of formal glucose tolerance testing, which takes two hours to complete. According to the current definition, two fasting glucose measurements above 126 mg/dL (7.0 mmol/l) is considered diagnostic for diabetes mellitus.
Patients with fasting glucose levels from 100 to 125 mg/dL (6.1 and 7.0 mmol/l) are considered to have impaired fasting glucose. Patients with plasma glucose at or above 140 mg/dL or 7.8 mmol/l, but not over 200, two hours after a 75 g oral glucose load are considered to have impaired glucose tolerance. Of these two pre-diabetic states, the latter in particular is a major risk factor for progression to full-blown diabetes mellitus as well as cardiovascular disease.[20]
While not used for diagnosis, an elevated level of glucose irreversibly bound to hemoglobin (termed glycosylated hemoglobin or HbA1c) of 6.0% or higher (the 2003 revised U.S. standard) is considered abnormal by most labs; HbA1c is primarily used as a treatment-tracking test reflecting average blood glucose levels over the preceding 90 days (approximately) which is the average lifetime of red blood cells which contain hemoglobin in most patients. However, some physicians may order this test at the time of diagnosis to track changes over time. The current recommended goal for HbA1c in patients with diabetes is <7.0%, which is considered good glycemic control, although some guidelines are stricter (<6.5%). People with diabetes who have HbA1c levels within this range have a significantly lower incidence of complications from diabetes, including retinopathy anddiabetic nephropathy.[21][22]
Screening
Diabetes screening is recommended for many people at various stages of life, and for those with any of several risk factors. The screening test varies according to circumstances and local policy, and may be a random blood glucose test, a fasting blood glucose test, a blood glucose test two hours after 75 g of glucose, or an even more formal glucose tolerance test. Many healthcare providers recommend universal screening for adults at age 40 or 50, and often periodically thereafter. Earlier screening is typically recommended for those with risk factors such as obesity, family history of diabetes, high-risk ethnicity (Hispanic, Native American, Afro-Caribbean, Pacific Islander).[23][24]
Many medical conditions are associated with diabetes and warrant screening. A partial list includes: high blood pressure, elevated cholesterol levels, coronary artery disease, past gestational diabetes, polycystic ovary syndrome, chronic pancreatitis, fatty liver, hemochromatosis, cystic fibrosis, several mitochondrial neuropathies and myopathies,myotonic dystrophy, Friedreich's ataxia, some of the inherited forms of neonatal hyperinsulinism. The risk of diabetes is higher with chronic use of several medications, including high-dose glucocorticoids, some chemotherapy agents (especially L-asparaginase), as well as some of the antipsychotics and mood stabilizers (especially phenothiazines and some atypical antipsychotics).
People with a confirmed diagnosis of diabetes are tested routinely for complications. This includes yearly urine testing for microalbuminuria and examination of the retina of the eye for retinopathy.
Prevention
Type 1 diabetes risk is known to depend upon a genetic predisposition based on HLA types (particularly types DR3 and DR4), an unknown environmental trigger (suspected to be an infection, although none has proven definitive in all cases), and an uncontrolled autoimmune response that attacks the insulin producing beta cells.[25] Some research has suggested that breastfeeding decreased the risk in later life;[26][27] various other nutritional risk factors are being studied, but no firm evidence has been found.[28] Giving children 2000 IU of Vitamin D during their first year of life is associated with reduced risk of type 1 diabetes, though the causal relationship is obscure.[29]
Children with antibodies to beta cell proteins (ie at early stages of an immune reaction to them) but no overt diabetes, and treated with vitamin B-3 (niacin), had less than half the diabetes onset incidence in a 7-year time span as did the general population, and an even lower incidence relative to those with antibodies as above, but who received no vitamin B3.[30]
Type 2 diabetes risk can be reduced in many cases by making changes in diet and increasing physical activity.[31][32] The American Diabetes Association (ADA) recommends maintaining a healthy weight, getting at least 2½ hours of exercise per week (several brisk sustained walks appear sufficient), having a modest fat intake, and eating sufficient fiber (eg, from whole grains). The ADA does not recommend alcohol consumption as a preventive, but it is interesting to note that moderate alcohol intake may reduce the risk (though heavy consumption absolutely and clearly increases damage to bodily systems significantly); a similarly confused connection between low dose alcohol consumption and heart disease is termed the French Paradox.
There is inadequate evidence that eating foods of low glycemic index is clinically helpful despite recommendations and suggested diets emphasizing this approach.[33]
There are numerous studies which suggest connections between some aspects of Type II diabetes with ingestion of certain foods or with some drugs. Some studies have shown delayed progression to diabetes in predisposed patients through prophylactic use of metformin,[32] rosiglitazone,[34] or valsartan.[35] In patients on hydroxychloroquine forrheumatoid arthritis, incidence of diabetes was reduced by 77% though causal mechanisms are unclear.[36] Breastfeeding may also be associated with the prevention of type 2 of the disease in mothers.[37] Clear evidence for these and any of many other connections between foods and supplements and diabetes is sparse to date; none, despite secondary claims for (or against), is sufficiently well established to justify as a standard clinical approach.
Treatment and management
Diabetes mellitus is currently a chronic disease, without a cure, and medical emphasis must necessarily be on managing/avoiding possible short-term as well as long-term diabetes-related problems. There is an exceptionally important role for patient education, dietetic support, sensible exercise, self monitoring of blood glucose, with the goal of keeping both short-term blood glucose levels, and long term levels as well, within acceptable bounds. Careful control is needed to reduce the risk of long term complications. This is theoretically achievable with combinations of diet, exercise and weight loss (type 2), various oral diabetic drugs (type 2 only), and insulin use (type 1 and for type 2 not responding to oral medications, mostly those with extended duration diabetes). In addition, given the associated higher risks of cardiovascular disease, lifestyle modifications should be undertaken to control blood pressure[38] and cholesterol by exercising more, smoking less or ideally not at all, consuming an appropriate diet, wearing diabetic socks, wearing diabetic shoes, and if necessary, taking any of several drugs to reduce blood pressure. Many type 1 treatments include combination use of regular or NPH insulin, and/or synthetic insulin analogs (eg, Humalog, Novolog or Apidra) in combinations such as Lantus/Levemir and Humalog, Novolog or Apidra. Another type 1 treatment option is the use of the insulin pump (eg, from Deltec Cozmo, Animas, Medtronic Minimed, Insulet Omnipod, or ACCU-CHEK). A blood lancet is used to pierce the skin (typically of a finger), in order to draw blood to test it for sugar levels.
In countries using a general practitioner system, such as the United Kingdom, care may take place mainly outside hospitals, with hospital-based specialist care used only in case of complications, difficult blood sugar control, or research projects. In other circumstances, general practitioners and specialists share care of a patient in a team approach.Optometrists, podiatrists/chiropodists, dietitians, physiotherapists, nursing specialists (eg, DSNs (Diabetic Specialist Nurse)), nurse practitioners, or Certified Diabetes Educators, may jointly provide multidisciplinary expertise. In countries where patients must provide their own health care (i.e., in the developed world, the US, and in much of the undeveloped world), the impact of out-of-pocket costs of adequate diabetic care can be very high. In addition to the medications and supplies needed, patients are often advised to receive regular consultation from a physician (e.g., at least every three to six months).
Peer support links people living with diabetes. Within peer support, people with a common illness share knowledge and experience that others, including many health workers, do not have. Peer support is frequent, ongoing, accessible and flexible and can take many forms—phone calls, text messaging, group meetings, home visits, and even grocery shopping. It complements and enhances other health care services by creating the emotional, social and practical assistance necessary for managing disease and staying healthy.
Cure
Cures for type 1 diabetes
There is no practical cure, at this time, for type 1 diabetes. The fact that type 1 diabetes is due to the failure of one of the cell types of a single organ with a relatively simple function (i.e. the failure of the beta cells in the Islets of Langerhans) has led to the study of several possible schemes to cure this form of diabetes mostly by replacing the pancreas or just the beta cells.[39] Only those type 1 diabetics who have received either a pancreas or a kidney-pancreas transplant (often when they have developed diabetic kidney disease (ie, nephropathy) and become insulin-independent) may now be considered "cured" from their diabetes. A simultaneous pancreas-kidney transplant is a promising solution, showing similar or improved survival rates over a kidney transplant alone.[40] Still, they generally remain on long-term immunosuppressive drugs and there is a possibility that the immune system will mount a host versus graft response against the transplanted organ.[39]
Transplants of exogenous beta cells have been performed experimentally in both mice and humans, but this measure is not yet practical in regular clinical practice partly due to the limited number of beta cell donors. Thus far, like any such transplant, it has provoked an immune reaction and long-term immunosuppressive drugs have been needed to protect the transplanted tissue.[41] An alternative technique has been proposed to place transplanted beta cells in a semi-permeable container, isolating and protecting them from the immune system. Stem cell research has also been suggested as a potential avenue for a cure since it may permit regrowth of Islet cells which are genetically part of the treated individual, thus perhaps eliminating the need for immuno-suppressants.[39] This new method, autologous nonmyeloablative HSTC, was recently developed by a research team comprised of scientists from the US and Brazil. This was originally tested in mice and in 2007 there was the first trial with fifteen patients. Recently this trial was continued and 8 more patients were added. In the trial, the researchers implanted diabetes type 1 patients with their own stem cells raised from their own bone marrow. The stem cell transplant led to an appreciable repopulation of functioning insulin-producing beta cells in the pancreas so the patients became insulin free. Most of these patients became insulin independent for a mean period of 18.8 months. At the present time, autologous nonmyeloablative HSCT remains the only treatment capable of reversing type 1 DM in humans.[42]
Microscopic or nanotechnological approaches are under investigation as well, in one proposed case with implanted stores of insulin metered out by a rapid response valve sensitive to blood glucose levels. At least two approaches have been demonstrated in vitro. These are, in some sense, closed-loop insulin pumps.
Cures for type 2 diabetes
Type 2 has had no definitive cure, although recently it has been shown that a type of gastric bypass surgery can normalize blood glucose levels in 80-100% of severely obese patients with diabetes. The precise causal mechanisms are being intensively researched; its results are not simply attributable to weight loss, as the improvement in blood sugars precedes any change in body mass. This approach may become a standard treatment for some people with type 2 diabetes in the relatively near future.[43] This surgery has the additional benefit of reducing the death rate from all causes by up to 40% in severely obese people.[44] A small number of normal to moderately obese patients with type 2 diabetes have successfully undergone similar operations.[45][46]
Prognosis
Patient education, understanding, and participation is vital since the complications of diabetes are far less common and less severe in people who have well-controlled blood sugar levels.[47][48] Wider health problems accelerate the deleterious effects of diabetes. These include smoking, elevated cholesterol levels, obesity, high blood pressure, and lack of regular exercise. According to a study, women with high blood pressure have a threefold risk of developing diabetes.
Anecdotal evidence suggests that some of those with type 2 diabetes who exercise regularly, lose weight, and eat healthy diets may be able to keep some of the disease or some of the effects of the disease in 'remission.' Certainly these tips can help prevent people predisposed to type 2 diabetes and those at pre-diabetic stages from actually developing the disorder as it helps restore insulin sensitivity. However patients should talk to their doctors about this for real expectations before undertaking it (esp. to avoid hypoglycemia or other complications); few people actually seem to go into total 'remission,' but some may find they need less of their insulin medications since the body tends to have lower insulin requirements during and shortly following exercise. Regardless of whether it works that way or not for an individual, there are certainly other benefits to this healthy lifestyle for both diabetics and nondiabetics.
The way diabetes is managed changes with age. Insulin production decreases because of age-related impairment of pancreatic beta cells. Additionally, insulin resistance increases because of the loss of lean tissue and the accumulation of fat, particularly intra-abdominal fat, and the decreased tissue sensitivity to insulin. Glucose tolerance progressively declines with age, leading to a high prevalence of type 2 diabetes and postchallenge hyperglycemia in the older population.[49] Age-related glucose intolerance in humans is often accompanied by insulin resistance, but circulating insulin levels are similar to those of younger people.[50] Treatment goals for older patients with diabetes vary with the individual, and take into account health status, as well as life expectancy, level of dependence, and willingness to adhere to a treatment regimen.[51]
Acute complications
- Diabetic ketoacidosis
Diabetic ketoacidosis (DKA) is an acute and dangerous complication that is always a medical emergency. Low insulin levels cause the liver to turn to fat for fuel (ie, ketosis);ketone bodies are intermediate substrates in that metabolic sequence. This is normal when periodic, but can become a serious problem if sustained. Elevated levels of ketone bodies in the blood decrease the blood's pH, leading to DKA. On presentation at hospital, the patient in DKA is typically dehydrated, and breathing rapidly and deeply. Abdominal pain is common and may be severe. The level of consciousness is typically normal until late in the process, when lethargy may progress to coma. Ketoacidosis can easily become severe enough to cause hypotension, shock, and death. Urine analysis will reveal significant levels of ketone bodies (which have exceeded their renal threshold blood levels to appear in the urine, often before other overt symptoms). Prompt, proper treatment usually results in full recovery, though death can result from inadequate or delayed treatment, or from complications (eg, brain edema). DKA is always a medical emergency and requires medical attention. Ketoacidosis is much more common in type 1 diabetes than type 2.
- Hyperglycemia hyperosmolar state
Hyperosmolar nonketotic state (HNS) is an acute complication sharing many symptoms with DKA, but an entirely different origin and different treatment. A person with very high (usually considered to be above 300 mg/dl (16 mmol/l)) blood glucose levels, water is osmotically drawn out of cells into the blood and the kidneys eventually begin to dump glucose into the urine. This results in loss of water and an increase in blood osmolarity. If fluid is not replaced (by mouth or intravenously), the osmotic effect of high glucose levels, combined with the loss of water, will eventually lead to dehydration. The body's cells become progressively dehydrated as water is taken from them and excreted. Electrolyte imbalances are also common and are always dangerous. As with DKA, urgent medical treatment is necessary, commonly beginning with fluid volume replacement. Lethargy may ultimately progress to a coma, though this is more common in type 2 diabetes than type 1.
- Hypoglycemia
Hypoglycemia, or abnormally low blood glucose, is an acute complication of several diabetes treatments. It is rare otherwise, either in diabetic or non-diabetic patients. The patient may become agitated, sweaty, and have many symptoms of sympathetic activation of the autonomic nervous system resulting in feelings akin to dread and immobilized panic. Consciousness can be altered or even lost in extreme cases, leading to coma, seizures, or even brain damage and death. In patients with diabetes, this may be caused by several factors, such as too much or incorrectly timed insulin, too much or incorrectly timed exercise (exercise decreases insulin requirements) or not enough food (specifically glucose containing carbohydrates). The variety of interactions makes cause identification difficult in many instances.
It is more accurate to note that iatrogenic hypoglycemia is typically the result of the interplay of absolute (or relative) insulin excess and compromised glucose counterregulation in type 1 and advanced type 2 diabetes. Decrements in insulin, increments in glucagon, and, absent the latter, increments in epinephrine are the primary glucose counterregulatory factors that normally prevent or (more or less rapidly) correct hypoglycemia. In insulin-deficient diabetes (exogenous) insulin levels do not decrease as glucose levels fall, and the combination of deficient glucagon and epinephrine responses causes defective glucose counterregulation.
Furthermore, reduced sympathoadrenal responses can cause hypoglycemia unawareness. The concept of hypoglycemia-associated autonomic failure (HAAF) in diabetes posits that recent incidents of hypoglycemia causes both defective glucose counterregulation and hypoglycemia unawareness. By shifting glycemic thresholds for the sympathoadrenal (including epinephrine) and the resulting neurogenic responses to lower plasma glucose concentrations, antecedent hypoglycemia leads to a vicious cycle of recurrent hypoglycemia and further impairment of glucose counterregulation. In many cases (but not all), short-term avoidance of hypoglycemia reverses hypoglycemia unawareness in affected patients, although this is easier in theory than in clinical experience.
In most cases, hypoglycemia is treated with sugary drinks or food. In severe cases, an injection of glucagon (a hormone with effects largely opposite to those of insulin) or anintravenous infusion of dextrose is used for treatment, but usually only if the person is unconscious. In any given incident, glucagon will only work once as it uses stored liver glycogen as a glucose source; in the absence of such stores, glucagon is largely ineffective. In hospitals, intravenous dextrose is often used.
Chronic complications
- Vascular disease
Chronic elevation of blood glucose level leads to damage of blood vessels (angiopathy). The endothelial cells lining the blood vessels take in more glucose than normal, since they don't depend on insulin. They then form more surface glycoproteins than normal, and cause the basement membrane to grow thicker and weaker. In diabetes, the resulting problems are grouped under "microvascular disease" (due to damage to small blood vessels) and "macrovascular disease" (due to damage to the arteries).
The damage to small blood vessels leads to a microangiopathy, which can cause one or more of the following:
- Diabetic retinopathy, growth of friable and poor-quality new blood vessels in the retina as well as macular edema (swelling of the macula), which can lead to severe vision loss or blindness. Retinal damage (from microangiopathy) makes it the most common cause of blindness among non-elderly adults in the US.
- Diabetic neuropathy, abnormal and decreased sensation, usually in a 'glove and stocking' distribution starting with the feet but potentially in other nerves, later often fingers and hands. When combined with damaged blood vessels this can lead to diabetic foot (see below). Other forms of diabetic neuropathy may present as mononeuritis or autonomic neuropathy. Diabetic amyotrophy is muscle weakness due to neuropathy.
- Diabetic nephropathy, damage to the kidney which can lead to chronic renal failure, eventually requiring dialysis. Diabetes mellitus is the most common cause of adult kidney failure worldwide in the developed world.
- Diabetic cardiomyopathy, damage to the heart, leading to diastolic dysfunction and eventually heart failure.
Macrovascular disease leads to cardiovascular disease, to which accelerated atherosclerosis is a contributor:
- Coronary artery disease, leading to angina or myocardial infarction ("heart attack")
- Stroke (mainly the ischemic type)
- Peripheral vascular disease, which contributes to intermittent claudication (exertion-related leg and foot pain) as well as diabetic foot.
- Diabetic myonecrosis ('muscle wasting')
Diabetic foot, often due to a combination of sensory neuropathy (numbness or insensitivity) and vascular damage, increases rates of skin ulcers and infection and, in serious cases, necrosis and gangrene. It is why diabetics are prone to leg and foot infections and why it takes longer for them to heal from leg and foot wounds. It is the most common cause of non-traumatic adult amputation, usually of toes and or feet, in the developed world.
Carotid artery stenosis does not occur more often in diabetes, and there appears to be a lower prevalence of abdominal aortic aneurysm. However, diabetes does cause higher morbidity, mortality and operative risks with these conditions.[52]
Diabetic encephalopathy[53] is the increased cognitive decline and risk of dementia observed in diabetes. Various mechanisms are proposed, including alterations to the vascular supply of the brain and the interaction of insulin with the brain itself.[54].
Epidemiology
In 2000, according to the World Health Organization, at least 171 million people worldwide suffer from diabetes, or 2.8% of the population.[55] Its incidence is increasing rapidly, and it is estimated that by the year 2030, this number will almost double.[55] Diabetes mellitus occurs throughout the world, but is more common (especially type 2) in the more developed countries. The greatest increase in prevalence is, however, expected to occur in Asia and Africa, where most patients will probably be found by 2030.[55] The increase in incidence of diabetes in developing countries follows the trend of urbanization and lifestyle changes, perhaps most importantly a "Western-style" diet. This has suggested an environmental (i.e., dietary) effect, but there is little understanding of the mechanism(s) at present, though there is much speculation, some of it most compellingly presented.[55]
For at least 20 years, diabetes rates in North America have been increasing substantially. In 2008 there were about 24 million people with diabetes in the United States alone, from those 5.7 million people remain undiagnosed. Other 57 million people are estimated to have pre-diabetes.[56]
The Centers for Disease Control has termed the change an epidemic.[57] The National Diabetes Information Clearinghouse estimates that diabetes costs $132 billion in the United States alone every year. About 5%–10% of diabetes cases in North America are type 1, with the rest being type 2. The fraction of type 1 in other parts of the world differs; this is probably due to both differences in the rate of type 1 and differences in the rate of other types, most prominently type 2. Most of this difference is not currently understood. The American Diabetes Association cite the 2003 assessment of the National Center for Chronic Disease Prevention and Health Promotion (Centers for Disease Control and Prevention) that 1 in 3 Americans born after 2000 will develop diabetes in their lifetime.[58][59]
According to the American Diabetes Association, approximately 18.3% (8.6 million) of Americans age 60 and older have diabetes.[60] Diabetes mellitus prevalence increases with age, and the numbers of older persons with diabetes are expected to grow as the elderly population increases in number. The National Health and Nutrition Examination Survey (NHANES III) demonstrated that, in the population over 65 years old, 18% to 20% have diabetes, with 40% having either diabetes or its precursor form of impaired glucose tolerance.[49]
Indigenous populations in first world countries have a higher prevalence and increasing incidence of diabetes than their corresponding non-indigenous populations. In Australia the age-standardised prevalence of self-reported diabetes in Indigenous Australians is almost 4 times that of non-indigenous Australians.[61] Preventative community health programs such as Sugar Man (diabetes education) are showing some success in tackling this problem.
History
The term diabetes (Greek: d?aß?t??, diabetes) was coined by Aretaeus of Cappadocia. It was derived from the Greek verb d?aßa??e??, diabaínein, itself formed from the prefix dia-, "across, apart," and the verb bainein, "to walk, stand." The verb diabeinein meant "to stride, walk, or stand with legs asunder"; hence, its derivative diabetes meant "one that straddles," or specifically "a compass, siphon." The sense "siphon" gave rise to the use of diabetes as the name for a disease involving the discharge of excessive amounts of urine. Diabetes is first recorded in English, in the form diabete, in a medical text written around 1425. In 1675, Thomas Willis added the word mellitus, from the Latin meaning "honey", a reference to the sweet taste of the urine. This sweet taste had been noticed in urine by the ancient Greeks, Chinese, Egyptians, Indians, and Persians. In 1776,Matthew Dobson confirmed that the sweet taste was because of an excess of a kind of sugar in the urine and blood of people with diabetes.[62]
Diabetes mellitus appears to have been a death sentence in the ancient era. Hippocrates makes no mention of it, which may indicate that he felt the disease was incurable. Aretaeus did attempt to treat it but could not give a good prognosis; he commented that "life (with diabetes) is short, disgusting and painful."[63]
Sushruta (6th century BCE) identified diabetes and classified it as Medhumeha.[64] He further identified it with obesity and sedentary lifestyle, advising exercises to help cure it.[64] The ancient Indians tested for diabetes by observing whether ants were attracted to a person's urine, and called the ailment "sweet urine disease" (Madhumeha). The Korean, Chinese, and Japanese words for diabetes are based on the same ideographs (???) which mean "sugar urine disease". In medieval Persia, Avicenna (980-1037) provided a detailed account on diabetes mellitus in The Canon of Medicine, "describing the abnormal appetite and the collapse of sexual functions and he documented the sweet taste of diabetic urine." Like Aretaeus before him, Avicenna recognized a primary and secondary diabetes. He also described diabetic gangrene, and treated diabetes using a mixture of lupine, trigonella (fenugreek), and zedoary seed, which produces a considerable reduction in the excretion of sugar, a treatment which is still prescribed in modern times. Avicenna also "described diabetes insipidus very precisely for the first time", though it was later Johann Peter Frank (1745-1821) who first differentiated between diabetes mellitus and diabetes insipidus.[65]
Although diabetes has been recognized since antiquity, and treatments of various efficacy have been known in various regions since the Middle Ages, and in legend for much longer, pathogenesis of diabetes has only been understood experimentally since about 1900.[66] The discovery of a role for the pancreas in diabetes is generally ascribed toJoseph von Mering and Oskar Minkowski, who in 1889 found that dogs whose pancreas was removed developed all the signs and symptoms of diabetes and died shortly afterwards.[67] In 1910, Sir Edward Albert Sharpey-Schafer suggested that people with diabetes were deficient in a single chemical that was normally produced by the pancreas—he proposed calling this substance insulin, from the Latin insula, meaning island, in reference to the insulin-producing islets of Langerhans in the pancreas.[66]
The endocrine role of the pancreas in metabolism, and indeed the existence of insulin, was not further clarified until 1921, when Sir Frederick Grant Banting and Charles Herbert Best repeated the work of Von Mering and Minkowski, and went further to demonstrate they could reverse induced diabetes in dogs by giving them an extract from the pancreatic islets of Langerhans of healthy dogs.[68] Banting, Best, and colleagues (especially the chemist Collip) went on to purify the hormone insulin from bovine pancreases at theUniversity of Toronto. This led to the availability of an effective treatment—insulin injections—and the first patient was treated in 1922. For this, Banting and laboratory director MacLeod received the Nobel Prize in Physiology or Medicine in 1923; both shared their Prize money with others in the team who were not recognized, in particular Best and Collip. Banting and Best made the patent available without charge and did not attempt to control commercial production. Insulin production and therapy rapidly spread around the world, largely as a result of this decision. Banting is honored by World Diabetes Day which is held on his birthday, November 14.
The distinction between what is now known as type 1 diabetes and type 2 diabetes was first clearly made by Sir Harold Percival (Harry) Himsworth, and published in January 1936.[69]
Despite the availability of treatment, diabetes has remained a major cause of death. For instance, statistics reveal that the cause-specific mortality rate during 1927 amounted to about 47.7 per 100,000 population in Malta.[70]
Other landmark discoveries include:[66]
- identification of the first of the sulfonylureas in 1942
- reintroduction of the use of biguanides for Type 2 diabetes in the late 1950s. The initial phenformin was withdrawn worldwide (in the U.S. in 1977) due to its potential for sometimes fatal lactic acidosis and metformin was first marketed in France in 1979, but not until 1994 in the US.
- the determination of the amino acid sequence of insulin (by Sir Frederick Sanger, for which he received a Nobel Prize)
- the radioimmunoassay for insulin, as discovered by Rosalyn Yalow and Solomon Berson (gaining Yalow the 1977 Nobel Prize in Physiology or Medicine)[71]
- the three-dimensional structure of insulin (PDB 2INS)
- Dr Gerald Reaven's identification of the constellation of symptoms now called metabolic syndrome in 1988
- demonstration that intensive glycemic control in type 1 diabetes reduces chronic side effects more as glucose levels approach 'normal' in a large longitudinal study,[72] and also in type 2 diabetics in other large studies
- identification of the first thiazolidinedione as an effective insulin sensitizer during the 1990s
In 1980, U.S. biotech company Genentech developed human insulin. The insulin is isolated from genetically altered bacteria (the bacteria contain the human gene for synthesizing human insulin), which produce large quantities of insulin. Scientists then purify the insulin and distribute it to pharmacies for use by diabetes patients.
Social issues
The 1990 "St Vincent Declaration"[73][74] was the result of international efforts to improve the care accorded to those with diabetes. Doing so is important both in terms of quality of life and life expectancy but also economically - expenses due to diabetes have been shown to be a major drain on health - and productivity-related resources for healthcare systems and governments.
Several countries established more and less successful national diabetes programmes to improve treatment of the disease.[75]
A study shows that diabetic patients with neuropathic symptoms such as numbness or tingling in feet or hands are twice more likely to be unemployed than those without the symptoms.[76]
See also
References
- ^ "Diabetes Blue Circle Symbol". International Diabetes Federation. 17 March 2006.
- ^ L M Tierney, S J McPhee, M A Papadakis (2002). Current medical Diagnosis & Treatment. International edition. New York: Lange Medical Books/McGraw-Hill. pp. 1203–1215. ISBN 0-07-137688-7.
- ^ a b c Rother, KI (2007). "Diabetes Treatment — Bridging the Divide". N Engl J Med 356 (15): 1499–1501. doi:. PMID 17429082.
- ^ a b c World Health Organisation Department of Noncommunicable Disease Surveillance (1999). "Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications" (PDF).
- ^ Mailloux, Lionel (2007-02-13). "UpToDate Dialysis in diabetic nephropathy". UpToDate. Retrieved on 2007-12-07.
- ^ "Other "types" of diabetes". American Diabetes Association. August 25, 2005.
- ^ "Diseases: Johns Hopkins Autoimmune Disease Research Center". Retrieved on 2007-09-23.
- ^ "FDA Approves First Ever Inhaled Insulin Combination Product for Treatment of Diabetes". Retrieved on 2007-09-09.
- ^ "MannKind Unveils Proposed Trade Name at Dedication of Danbury Manufacturing Facility". Retrieved on 2008-10-23.
- ^ Baillie, K (2008-07-05). "ClinicLog article on current diabetes trials.". ClinicLog.com. Retrieved on 2008-07-23.
- ^ Eberhart, MS; Ogden C, Engelgau M, Cadwell B, Hedley AA, Saydah SH (19 November 2004). "Prevalence of Overweight and Obesity Among Adults with Diagnosed Diabetes --- United States, 1988--1994 and 1999--2002". Morbidity and Mortality Weekly Report (Centers for Disease Control and Prevention) 53 (45): 1066–1068. Retrieved on 2007-03-11.
- ^ Arlan Rosenbloom, Janet H Silverstein (2003). Type 2 Diabetes in Children and Adolescents: A Clinician's Guide to Diagnosis, Epidemiology, Pathogenesis, Prevention, and Treatment. American Diabetes Association,U.S.. pp. 1. ISBN 978-1580401555.
- ^ Lang, Iain A.; Tamara S. Galloway, Alan Scarlett, William E. Henley, Michael Depledge, Robert B. Wallace, and David Melzer (2008). "Association of Urinary Bisphenol A Concentration with Medical Disorders and Laboratory Abnormalities in Adults". Journal of the American Medical Association 300 (1): 1303–1310. doi:.
- ^ "Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group". Lancet 352 (9131): 854–65. 1998. doi:. PMID 9742977.
- ^ Lawrence JM, Contreras R, Chen W, Sacks DA (May 2008). "Trends in the prevalence of preexisting diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women, 1999-2005". Diabetes Care 31 (5): 899–904. doi:. PMID 18223030.
- ^ Lyssenko, V. (2008). "Clinical risk factors, DNA variants, and the development of type 2 diabetes". N Engl J Med 359 (21): 2220–2232. doi:.
- ^ Walley AJ, Blakemore AI, Froguel P (2006). "Genetics of obesity and the prediction of risk for health". Hum. Mol. Genet. 15 Spec No 2: R124–30. doi:. PMID 16987875.
- ^ "Monogenic Forms of Diabetes: Neonatal Diabetes Mellitus and Maturity-onset Diabetes of the Young". National Diabetes Information Clearinghouse (NDIC) (National Institute of Diabetes and Digestive and Kidney Diseases, NIH). Retrieved on 2008-08-04.
- ^ Barrett TG (2001). "Mitochondrial diabetes, DIDMOAD and other inherited diabetes syndromes". Best Pract. Res. Clin. Endocrinol. Metab. 15 (3): 325–43. doi:. PMID 11554774.
- ^ Santaguida PL, Balion C, Hunt D, Morrison K, Gerstein H, Raina P, Booker L, Yazdi H. "Diagnosis, Prognosis, and Treatment of Impaired Glucose Tolerance and Impaired Fasting Glucose". Summary of Evidence Report/Technology Assessment, No. 128. Agency for Healthcare Research and Quality. Retrieved on 2008-07-20.
- ^ Sniderman, AD; Bhopal R, Prabhakaran D, Sarrafzadegan N, Tchernof A (2007). "Why might South Asians be so susceptible to central obesity and its atherogenic consequences? The adipose tissue overflow hypothesis". International journal of epidemiology 36 (1): 220–225. doi:. PMID 17510078.
- ^ Genuth S (Jan-Feb 2006). "Insights from the diabetes control and complications trial/epidemiology of diabetes interventions and complications study on the use of intensive glycemic treatment to reduce the risk of complications of type 1 diabetes". Endocr Pract 12 (Suppl 1): 34–41. ISSN 1530-891X. PMID 16627378.
- ^ Lee CM, Huxley RR, Lam TH, Martiniuk AL, Ueshema H, Pan WH, Welborn T, Woodward M; Asia Pacific Cohort Studies Collaboration (2007). "Prevalence of diabetes mellitus and population attributable fractions for coronary heart disease and stroke mortality in the WHO South-East Asia and Western Pacific regions". Asia Pac J Clin Nutr 16 (1): 187–92. PMID 17215197.
- ^ Seidell JC (2000). "Obesity, insulin resistance and diabetes--a worldwide epidemic". Br. J. Nutr. 83 Suppl 1: S5–8. PMID 10889785.
- ^ Daneman D (2006). "Type 1 diabetes". Lancet 367 (9513): 847–58. doi:. PMID 16530579.
- ^ Borch-Johnsen K, Joner G, Mandrup-Poulsen T, Christy M, Zachau-Christiansen B, Kastrup K, Nerup J (1984). "Relation between breast-feeding and incidence rates of insulin-dependent diabetes mellitus. A hypothesis". Lancet 2 (8411): 1083–6. doi:. PMID 6150150.
- ^ Naim Shehadeh, Raanan Shamir, Moshe Berant, Amos Etzioni (2001). "Insulin in human milk and the prevention of type 1 diabetes". Pediatric Diabetes 2 (4): 175–177. doi:.
- ^ Virtanen S, Knip M (2003). "Nutritional risk predictors of beta cell autoimmunity and type 1 diabetes at a young age". Am J Clin Nutr 78 (6): 1053–67. PMID 14668264.
- ^ Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM (2001). "Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study". Lancet 358: 1500. doi:. PMID 11705562.
- ^ Elliott RB, Pilcher CC, Fergusson DM, Stewart AW (Sep-Oct 1996). "A population based strategy to prevent insulin-dependent diabetes using nicotinamide". J. Pediatr. Endocrinol. Metab. 9 (5): 501–9.PMID 8961125.
- ^ Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson J, Hemiö K, Hämäläinen H, Härkönen P, Keinänen-Kiukaanniemi S, Laakso M, Louheranta A, Mannelin M, Paturi M, Sundvall J, Valle T, Uusitupa M, Tuomilehto J (2006). "Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study". Lancet 368 (9548): 1673–9. doi:. PMID 17098085.
- ^ a b Knowler W, Barrett-Connor E, Fowler S, Hamman R, Lachin J, Walker E, Nathan D (2002). "Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin". N Engl J Med 346 (6): 393–403. doi:. PMID 11832527.
- ^ Bantle JP, Wylie-Rosett J, Albright AL, et al (2006). "Nutrition recommendations and interventions for diabetes--2006: a position statement of the American Diabetes Association". Diabetes Care 29 (9): 2140–57. doi:. PMID 16936169.
- ^ Gerstein H, Yusuf S, Bosch J, Pogue J, Sheridan P, Dinccag N, Hanefeld M, Hoogwerf B, Laakso M, Mohan V, Shaw J, Zinman B, Holman R (2006). "Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial". Lancet 368 (9541): 1096–105. doi:. PMID 16997664.
- ^ Kjeldsen SE, Julius S, Mancia G, McInnes GT, Hua T, Weber MA, Coca A, Ekman S, Girerd X, Jamerson K, Larochelle P, Macdonald TM, Schmieder RE, Schork MA, Stolt P, Viskoper R, Widimsky J, Zanchetti A; for the VALUE Trial Investigators (2006). "Effects of valsartan compared to amlodipine on preventing type 2 diabetes in high-risk hypertensive patients: the VALUE trial". J Hypertens 24 (7): 1405–1412. doi:. PMID 16794491.
- ^ Wasko MC, Hubert HB, Lingala VB, et al (2007). "Hydroxychloroquine and risk of diabetes in patients with rheumatoid arthritis". JAMA 298 (2): 187–93. doi:. PMID 17622600.
- ^ Stuebe AM, Rich-Edwards JW, Willett WC, Manson JE, Michels KB (2005). "Duration of lactation and incidence of type 2 diabetes". JAMA 294 (20): 2601–10. doi:. PMID 16304074.
- ^ Adler, A.I.; Stratton, I. M.; Neil, H.A.; et al (2000). "Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study". BMJ 321 (7258): 412–419. doi:. PMID 10938049.
- ^ a b c Vinik AI, Fishwick DT, Pittenger G (2004). "Advances in diabetes for the millennium: toward a cure for diabetes". MedGenMed : Medscape general medicine 6 (3 Suppl): 12. PMID 15647717.
- ^ Stratta RJ, Alloway RR. (1998). "Pancreas transplantation for diabetes mellitus: a guide to recipient selection and optimum immunosuppression". BioDrugs. 10 (5): 347–357. doi:. PMID 18020607.
- ^ Shapiro AM, Ricordi C, Hering BJ, et al (2006). "International trial of the Edmonton protocol for islet transplantation". N. Engl. J. Med. 355 (13): 1318–30. doi:. PMID 17005949.
- ^ Couri, B., Oliveira, M., Stracieri, A., Moraes, D., Pieroni, F., Barros, G., et al. (2009). C-Peptide levels and insulin independence following autologous nonmyeloablative hematopoietic stem cell transplantation in newly diagnosed type 1 diabetes mellitus. Journal of the American Medical Association, 301(15), 1573-1579.
- ^ Rubino, F; Gagner M (2002). "Potential of surgery for curing type 2 diabetes mellitus". Ann. Surg. 236 (5): 554–9. doi:. PMID 12409659.
- ^ Adams, TD; Gress RE, Smith SC, et al (2007). "Long-term mortality after gastric bypass surgery". N. Engl. J. Med. 357 (8): 753–61. doi:. PMID 17715409.
- ^ Cohen, RV; Schiavon CA, Pinheiro JS, Correa JL, Rubino F (2007). "Duodenal-jejunal bypass for the treatment of type 2 diabetes in patients with body mass index of 22-34 kg/m2: a report of 2 cases".Surg Obes Relat Dis. 3 (2): 195–7. doi:. PMID 17386401.
- ^ Vasonconcelos, Alberto (2007-09-01). "Could type 2 diabetes be reversed using surgery?". New Scientist (2619): 11–13. Retrieved on 2007-09-26.
- ^ Nathan, D.M.; Cleary P.A., Backlund J.Y., et al (2005). "Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes". N. Engl. J. Med. 353 (25): 2643–53.doi:. PMID 16371630.
- ^ The Diabetes Control and Complications Trial Research Group (15 Apr 1995). "The effect of intensive diabetes therapy on the development and progression of neuropathy". Annals of Internal Medicine122 (8): 561–568. ISSN 0003-4819. PMID 7887548.
- ^ a b Harris MI, Flegal KM, Cowie CC, et al (1998). "Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988-1994". Diabetes Care 21 (4): 518–24. doi:. PMID 9571335.
- ^ Annette M. Chang and Jeffrey B. Halter (2003). "Aging and insulin secretion". AJP - Endocrinology and Metabolism. Retrieved on 2007-05-14.
- ^ "Diabetes and Aging". Diabetes Dateline. National Institute of Diabetes and Digestive and Kidney Diseases. 2002. Retrieved on 2007-05-14.
- ^ Weiss J, Sumpio B (2006). "Review of prevalence and outcome of vascular disease in patients with diabetes mellitus". Eur J Vasc Endovasc Surg 31 (2): 143–50. doi:. PMID 16203161.
- ^ Aristides Veves, Rayaz A. Malik (2007). Diabetic Neuropathy: Clinical Management (Clinical Diabetes), Second Edition. New York: Humana Press. pp. 188–198. ISBN 1-58-829626-1.
- ^ Gispen WH, Biessels GJ (November 2000). "Cognition and synaptic plasticity in diabetes mellitus". Trends Neurosci. 23 (11): 542–9. doi:. PMID 11074263.
- ^ a b c d Wild S, Roglic G, Green A, Sicree R, King H (May 2004). "Global prevalence of diabetes: estimates for the year 2000 and projections for 2030". Diabetes Care 27 (5): 1047–53.doi:. PMID 15111519.
- ^ hhttp://www.cdc.gov/Features/diabetesfactsheet/
- ^ "CDC's Diabetes Program - News and Information - Press Releases - October 26 2000". Retrieved on 2008-06-23.
- ^ Narayan K, Boyle J, Thompson T, Sorensen S, Williamson D (2003). "Lifetime risk for diabetes mellitus in the United States". JAMA 290 (14): 1884–90. doi:. PMID 14532317.
- ^ American Diabetes Association (2005). "Total Prevalence of Diabetes & Pre-diabetes". Retrieved on 2006-03-17.
- ^ "Seniors and Diabetes". Elderly And Diabetes - Diabetes and Seniors. LifeMed Media. 2006. Retrieved on 2007-05-14.
- ^ Australian Institute for Health and Welfare. "Diabetes, an overview". Retrieved on 2008-06-23.
- ^ Dobson, M. (1776). "Nature of the urine in diabetes". Medical Observations and Inquiries 5: 298–310.
- ^ Medvei (1993). History of Clinical Endocrinology. 23-34
- ^ a b Dwivedi, Girish & Dwivedi, Shridhar (2007). History of Medicine: Sushruta – the Clinician – Teacher par Excellence. National Informatics Centre (Government of India).
- ^ Nabipour, I. (2003), "Clinical Endocrinology in the Islamic Civilization in Iran", International Journal of Endocrinology and Metabolism 1: 43–45 [44–5]
- ^ a b c Patlak M (2002). "New weapons to combat an ancient disease: treating diabetes". Faseb J 16 (14): 1853. doi:. PMID 12468446.
- ^ Von Mehring J, Minkowski O. (1890). "Diabetes mellitus nach pankreasexstirpation". Arch Exp Pathol Pharmakol 26: 371–387. doi:.
- ^ Banting FG, Best CH, Collip JB, Campbell WR, Fletcher AA (01 Jan 1922). "Pancreatic extracts in the treatment of diabetes mellitus". Canad Med Assoc J 12 (10): 141–146. PMID 1933711.
- ^ Himsworth (1936). "Diabetes mellitus: its differentiation into insulin-sensitive and insulin-insensitive types". Lancet i: 127–130. doi:.
- ^ Department of Health (Malta), 1897–1972:Annual Reports.
- ^ Yalow RS, Berson SA (1960). "Immunoassay of endogenous plasma insulin in man". J. Clin. Invest. 39: 1157–75. doi:. PMID 13846364.
- ^ The Diabetes Control And Complications Trial Research Group, (1993). "The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group". N Engl J Med 329 (14): 977–86. doi:. PMID 8366922.
- ^ Theodore H. Tulchinsky, Elena A. Varavikova (2008). The New Public Health, Second Edition. New York: Academic Press. p. 200. ISBN 0-12-370890-7.
- ^ Piwernetz K, Home PD, Snorgaard O, Antsiferov M, Staehr-Johansen K, Krans M. (1993). "Monitoring the targets of the St Vincent Declaration and the implementation of quality management in diabetes care: the DIABCARE initiative. The DIABCARE Monitoring Group of the St Vincent Declaration Steering Committee.". Diabet Med. 10 (4): 303–4. PMID 8508624.
- ^ Dubois, HFW and Bankauskaite, V (2005). "Type 2 diabetes programmes in Europe" (PDF). Euro Observer 7 (2): 5–6.
- ^ Stewart WF, Ricci JA, Chee E, Hirsch AG, Brandenburg NA (2007). "Lost productive time and costs due to diabetes and diabetic neuropathic pain in the US workforce". J. Occup. Environ. Med. 49 (6): 672–9. doi:. PMID 17563611.
External links
- Diabetesat the Open Directory Project
- American Diabetes Association
- National Diabetes Education Program
Bizarre Patents Patent No. 6612440 Banana Protective Device A banana protective device for storing and transporting a banana carefully.
In other important medial fields such alcoholism there are bizzare patents such as the following one which relates generally to the treatment of alcoholism, and more particularly, to supplementing the diet with assimilable chelated chromium, for this purpose.
US Patent 5013752 - Prevention and treatment of alcoholism by the use of dietary chromium
Bizarre Patents
Description
1. Field of the Invention
This invention relates generally to the treatment of alcoholism, and more particularly, to supplementing the diet with assimilable chelated chromium, for this purpose.
The assimilation of an adequate quantity of physiologically important micronutrients is essential to the health of both humans and animals. Failure of the body to ingest and absorb the necessary amounts of essential micronutrients (e.g., vitamins and/or minerals) can lead to improper functioning of the metabolic processes as well as to a variety of diseases and associated symptoms. For example, anemia is correlated with an iron deficiency, and goiter is correlated with an iodine deficiency.
2. Description of Prior Art
Dr. Walter Merz of the Human Nutrition Laboratory in Bethesda, Md., was the first scientist to describe the occurrence and function of chromium in biological systems (Physiological Rev. 49:163, 1969). This was followed in 1970 by the proclamation of Dr. Henry A. Schroeder, Professor of Physiology Emeritus at the Darmouth Medical School, that chromium deficiency was a factor in atherosclerosis (Jour. Chronic Diseases 23:123). Regrettably, this knowledge was not then recognized, accepted, and applied to medical practice. Most recently, Gary W. Evans, PhD, and Muriel B. Gilman at Bemidji State University, Mont. 56601, have prepared a paper (for 1989 publication in one of the journals of the American Chemical Society) titled "Anabolic Effect of Chromium Picolinate". Therein they identify metabolic mechanisms showing how ingestion of naturally occurring chromium beneficially decreases LD ("bad") cholesterol and increases HD ("good") cholesterol in blood serum. They link these observations to "death from heart disease" and to treatment and prevention of diabetes.
3. Chromium Deficiency
Average Americans are at far greater risk for being afflicted with hypoglycemia and/or diabetes than most foreigners. This is because many have overindulged in sugar consumption (over 5 ounces/day) throughout their life times. They have thereby excessively reduced their reserve supplies of chromium in their bodies--amounts with which they were amply provided at birth. Comparison of chromium concentrations in the tissues of Americans and foreigners of all ages showed chromium to be present in all young bodies. It was not detected in 15-23 percent of tissues from Americans over 50 years old but was found in the bodies of almost every foreigner (98.5%). Estimates based on organ weights indicated that native Africans had twice, Near Easterners 4.4 times, and Orientals five times as much chromium in their bodies as did Americans (ref. Schroeder, p. 73). Blood chromium has not been shown to reflect tissue stores. Very few foods contain readily assimilable chromium compounds capable of replenishing bodies drained and depleted of essential GTF. The trace metal chromium-in its trivalent (Cr+++) chelated form, known as GTF (Glucose Tolerance Factor)--is indispensable for burning blood-sugar Since adequate synthesis of GTF in the human body is questionable, Dr. Pfeiffer declared that this compound be assigned full-fledged vitamin status. Pure GTF is completely nontoxic. Mothers--to protect their babies and give them a good start in life--sacrificially transfer much of the residual chromium in their bodies to their growing fetuses. Placental tissue has the highest measured level of chromium in the body. American women after several pregnancies usually exhibit greatly reduced Cr-levels in their bodies.
4. Alcoholism and Hypoglycemia
Other than the recognition by physicians and scientists that hypoglycemia (a glucose intolerance disease) consistently accompanies the disease of alcoholism, there was no prior identification in the medical literature of alcoholism as a consequence of chromium deficiency. In fact, a recent pertinent declaration by Dr. William Mayer, Assistant Secretary of Defense for Health and Welfare, and head of the premier American alcoholic research agency--the Alcoholic, Drug Abuse, and Mental Health Administration, Washington, D.C.--states (ref. Babor, p. 197):
"Then there are `magic bullets` such as insulin for diabetes, a drug that controls an otherwise devastating metabolic disease. We don't see signs of any such`miracle drug` in the field of treatment for alcoholics."
This invention denies the continuing validity of that statement.
5. Genetic and Psychological Factors
The existence of genetic predisposition to alcoholism is long established. It has a factual physiological basis. Mental illness as a factor is not eliminated; but, for most alcoholics, it can now be relegated to a minor role. The new knowledge disclosed by this invention allows us to affirm unequivocally: Craving for alcohol is NOT due to moral weakness. It is a sickness--the conditioned response of the body to a pathological lack in the diet of the essential trace element chromium.
SUMMARY OF THE INVENTION
I have discovered that the physiological disorder of alcoholism is due to the body's deficiency of the essential metal chromium. This pathological condition of chromic deficiency is herein called hypochromism. Based upon my discovery of the cause-and-effect relationship between hypochromism and alcoholism, I claim that the disease of alcoholism can be prevented and/or therapeutically cured by replenishing the body's depleted supply of the trace element chromium. This particular micronutrient is the most deficient of all micronutrients vitamins and minerals in the diet of Americans. The major cause of hypochromism is excessive consumption of sucrose (ordinary table sugar).
DETAILED DESCRIPTION
Applicant's familiarity with chromium deficiency (which results mostly from ingestion of sugar and/or glucose) and with its direct connection to cardiovascular disease as the major cause of death in this country stimulated further studies and medical observations. Results of these observations supplied the background information necessary for the conclusions presented in this disclosure.
Pertinent details of such background knowledge are next cited:
(a) Functional hypoglycemia (not due to dysfunction of glands) and adult-onset diabetes mellitis (hyperglycemia dysinsulinism) are the two most familiar manifestations of blood-sugar disorders (glucose intolerance). The delicate balance between these two abnormal states of health is maintained by GTF working with the hormones insulin (Pfeiffer, pp. 290-1) and glucagon.
(b) These disorders are caused by hypochromism (depleted supplies of chromium in the body). Alcoholism is here claimed and shown below to have the same cause. Beasley (p. 77) states: "Undoubtedly the commonest cause of hypoglycemia . . . is overindulgence in alcohol."
(c) Women are more subject to these intolerances than are men. These symptoms are regularly observed in parous women (those who have given birth to children). Pregnant women also commonly exhibit gestational diabetes (blood-sugar levels in excess of 120 mg %). For example, two young women in their eighth month of pregnancy exhibited blood-sugar levels of 140 mg % and 180 mg %. The first, after taking prescribed chromium supplements of 100 µg tablets (GTF complex from yeast), one with each meal for 10 days (a total of 30×100 µg=3000 µg=3 mg) dropped her glucose blood level down to 80 mg %, and the second expectant mother on the same prescription dropped her level down to 90 mg % in two weeks' time. The natural
(d) Carl C. Pfeiffer, PhD, MD, Director of condition for normal persons is to maintain a fasting level of 70 to 100 mg % of glucose in the blood. Princeton's Brain Bio Center, states (ref, p. 290): "Many women in Western countries are so deficient in chromium that the white blood cell chromium level may decrease by 50 percent with each pregnancy, resulting first in complete alcohol intolerance and later in glucose intolerance (adult-type diabetes).
(e) A pertinent statistic on alcoholism quoted by Beasley (ref, p. 30) is: "twice as many black women as black men report health problems due to drinking". This result follows qualitatively as a logical consequence from items (b), (c), and (d) above. The higher quantitive proportions (women/men=2:1) reflect primarily higher birth rates among the black population than among other racial groups, rather than necessarily indicate a higher rate of alcohol consumption among black than non-black cohorts.
BIOLOGICALLY AVAILABLE CHROMIUM
Ordinary foods consumed in the diet of average Americans contain such low levels and low quality of assimilable chromium that losses greatly exceed the intake of this needed metal for the reasons explained earlier (see paraqraph #3). The best-known natural source of nutritional chromium is brewer's yeast grown on blackstrap molasses. A better food supplement holding much higher levels of chelated chromium has been GTF Complex sold in healthfood stores. Most of the population of the Westernized world--the inhabitants of the industralized nations--are afflicted with chronic (slow-acting) hypochromism, reflected by cardiovascular and related diseases.
Alcoholism can be regarded as the manifestation of severely acute hypochromism. In this regard, there has been failure to recognize that sucrose acts as a chronic toxin by cumulatively extracting essential chromium from the body, thereby shortening life. The toxic effects of ingesting sucrose have been previously reported by J. P. Dobbins (J. Nat. Health Federation, Vol. 7, Nos. 3 and 4, 1988, and in the September 1987 publication Hypoclycemia. Violent Crime, and the Dangers of Sugar, Philosanus, 326 East Colorado Boulevard, Suite 103, Pasadena, Calif. 91101).
In accordance with the present invention, it has been found that chromium intake into the body can be accelerated and greatly increased by consumption of chromium picolinate, known commercially as CHROMAX II, as cited in U.S. Pat. Ser. No. 4,315,927, and sold by Nutrition 21. It is found naturally in the body and is characterized by a high rate of assimilation into the blood serum.
TREATMENT FOR ALCOHOLICS
The recommended simple procedure is to consume food supplement tablets of readily assimilable chelated chromium (earlier "GTF Complex", but now preferably high-potency GTF, the latest CHROMAX II) for a sufficient length of time to replenish the body's depleted reserve supply. This involves continuing the ingestion of GTF until the level of chromium in body tissues reaches or exceeds that present at birth--its highest point. For most Americans, this is a minimum of 21/2 parts per billion (ppb)--equivalent to a total of 1.4 mg in the body of a normal 70 kg Western adult or to a level of 12 ppb--equivalent to a total of 7 mg in the body of a mainland Chinese. The diagnostic procedure for determining this level is preferably by means of spectrographic hair analysis (see Passwater, pp. 24-25). Blood analysis is a less reliable, less meaningful, and less easily performed test than hair analysis. For an alcoholic, the cessation of his craving for ethanol is a good indicator that he has achieved minimum replacement of his needed stores. (He has in effect refilled his "overdrawn bank account", so that he is again capable of meeting normal daily demands of stress or anxiety without having to resort to the harmful temporary crutch of sugar or alcohol, or to the equivalent adrenaline-stimulating drugs, caffeine, theophylline, nicotine--in coffee, tea, or tobacco. These alkaloid drugs briefly elevate the blood-sugar levels, but their long-term effects are to act as depressants for the nervous system.)
Further, the presence of adequate reserve supplies of GTF in the body aids the opposite-acting pancreatic hormones insulin and glucagon to stabilize more rapidly the body's glucose blood level within its normal range of 70-100 mg/100 ml.
Accordingly, the method of preventing and/or therapeutically curing the disease of alcoholism comprises the step of supplementing the diet with biologically available chromium. Such chromium is most preferably chelated chromium, which may be synthetically-produced chromium picolinate. This is an orthomolecular (nondrug) medicine having the formula ##STR1## Such supplementing of the diet is continued until the blood glucose level is brought to normal or substantially normal level, as at birth. Such supplementing is typically carried out by ingesting a daily average amount of between about 150 and 250 micrograms of chelated chromium over a period of days until the blood glucose level is brought to normal or substantially normal level. The ingested chromium picolinate is preferably in compressed powder tablet or free powder capsule form.
There usually exists a large time-lag of about 10 to 20 years before new knowledge discovered by medical scientists about health and disease reaches the medical schools, is taught to aspiring physicians, and finally is applied in practice to benefit the general public. To illustrate this point, the so-called "bible of medicine", used as a standard reference book by physicians, and college text by medical students, is: Harrison's Principles of Internal Medicine, McGraw Hill. Its latest version (11th edition, 1988) in the section devoted to "Diabetes Mellitus and Hypoglycemia" makes no mention yet of chromium in relation thereto, nor is the common condition of gestational diabetes recognized. This same absence of important information about medical benefits of treating patients with nutrient chromium characterizes the competitive Textbook of Internal Medicine, edited by W. N. Kelley, M.D., and published by Lippincott Co. (1st edition 1989). J. D. Beasley on p. 12 of his 1987 book Wrong Diagnosis, Wrong Treatment: The Pliqht of the Alcoholic in America (publ. by Essential Medical Information Systems, Inc., N.Y.) identifies "alcoholism as a . . . genetic/metabolic disorder more closely related to diabetes than to any behavioral disorder" (emphasis added). Nowhere in his book is chromium mentioned. Had Walter Merz or Henry Schroeder about 15 years ago applied for and received a patent on the application of their knowledge to treat and/or cure sugar-related diseases, then this kind of therapy would possibly have become widespread by now, and much suffering could have been alleviated.
A final word applied to the subject of chromium deficiency is from Dr. Schroeder (page 84) who says: "Modern man makes many mistakes through lack of knowledge, but there is no excuse for his continuing his mistakes in the face of knowledge."
The herein method of preventing and/or therapeutically treating the disease of alcoholism, by supplementing the diet with synthetically produced nutrient chromium picolinate at levels of over 50 µg, (the minimum US RDA) also contemplates the provision of such chromium picolinate in a food bar now lacking any added chromium. Typical of such food bars are those 200-calorie bars used for weight control "providing 100% US RDA of 10 essential vitamins and 2 essential minerals plus significant amounts of 3 additional minerals and protein", as manufactured and sold by Nutrilite, division of Amway.
Quantity % U.S. RDA ___ Protein 10 g 15 VITAMINS Vitamin A 5,000 I.U. 100 Vitamin D 400 I.U. 100 Vitamin E 30 I.U. 100 Vitamin C 60 mg 100 Folic Acid 4 mg 100 Thiamine (B-1) 1.5 mg 100 Riboflavin (B-2) 1.7 mg 100 Niacin 20 mg 100 Vitamin B-6 2 mg 100 Vitamin B-12 6 mcg 100 MINERALS Calcium 3 g 30 Phosphorus 3 g 30 Iodine 150 mcg 100 Iron 18 mg 100 Magnesium 120 mg 30 Chromium Picolinate 100 µg 100
Ingredients: Higb Frutose Corn Syrup, Dehydrated Apples, Whey Protein, Textured Soy Flour, Fructose, Partially Hydrogenated Vegetable Oil (from Cotton, Soy, Palm, Palm Kernel), Soy Protein Isolate, Corn Bran, Natural Flavors, Vital Wheat Gluten-Dicalcium Phosphate, Non Fat Milk Solids, Cinnamon, Magnesium Oxide, Whey Solids, Lecithin, Ascorbic Acid, Ferrous Fumarate, Vitamin E Acetate, Sodium Caseinate, Niacinamide, Vitamin A, Palmitate, Vitamin B-12, Pyridoxine Hydrochloride, Riboflavin, Ethycellulose, Thiamine Mononitrate, Calcium Sulfate, Folic Acid, Potassium Iodine, Ergocalciferol.
A 100% water soluble form of chromium picolinate may be used in the food bar of the EXAMPLE. That soluble form is chromium picolinate complexed with hydroxypropyl Beta-cyclodextrine, and is produced by Nutrition 21, San Diego, Calif. It may be substituted in like amount for the chromium picolinate recited in the EXAMPLE. Each food bar as defined in the EXAMPLE preferably contains between about 100 and 250 µg of chromium picolinate, or that amount of chromium picolinate complexed with hydroxypropyl Betacyclodextrine.
The method of the invention also anticipates treating acute hypochromism parenterally, not through the alimentary canal (but rather by injection through some other route, as subcutaneous, intramuscular, intravenous, etc.) with an aqueous solution of chromic picolinate.
Inventor Dobbins, John P. Application: No. 509214 filed on 04/16/1990
US Classes and Field of Search: 514/505, 424/655, 426/306, 514/810, 514/811
Examiners Primary: Rose, Shep K. Assistant: Weddington, Kevin E.
US Patent References: 4006219, 4315927, 4543262, 4918102
Foreign Patent References: 8701285 WO. 03/09/1987
International Classes: A61K 033/24
Glucose Tolerance Factor (GTF) is a important component for diabetic people. Diabetes is recognized as a major global health problem. Diabetes affects 5%-10% of the population in developed countries. Diabetics suffer from lack of insulin or a deficiency in the body's ability to respond to insulin. Diabetes is a chronic illness with no cure and can lead to kidney failure, heart problems, strokes or blindness, as well as other complications.
http://www.blogcatalog.com/search.frame.php?term=gtf+chromium++Dr.Frank+Mao&id=fce45296e9aa7449fb5d66866ca52972
Sunday, October 26, 2008
The Depletion Of GTF Chromium
Dr Walter Mertz indicated that:
"Type II Diabetes is not a disease. It is due to the deficiency of a natural element known as GTF."
Prof Dr Frank Mao Chia-Hung, PhD in Endocrinology and a dairy product specialist, discovered that the causes of diabetes are:
" more than 80% - lack of GTF chromium
about 10% - lack of insulin receptor
between 5%-10% - lack of insulin. "
Most of the people, daily consume GTF chromium is less than 20% of those needed by our body. Furthermore our body is only able to absorb 05-2% of the GTF chromium that we consumed.
Insufficient intake of GTF chromium and excessive lost due to:
- aging
- obesity
- overwork
- low protein diet
- pregnancy
- surgery
- alcohol
- diseases
All those results in depletion of GTF chromium in our body.
According to Dr Stephen Davie's research report published in 1997, our bodies GTF chromium level declines with age.
When our body is lack of GTF chromium, glucose is unable to enter cells effectively. Glucose will accumulate in the blood vessels and result in a chain of health problems.
Using 180 people from Beijing, China, who had Type II diabetes, Richard Anderson, Ph.D., from the U.S. Department of Agriculture's Agriculture Research Service, proved that a daily 1,000 mcg (1 mg) dose of chromium picolinate could stabilize blood sugar in just two months. After four months of supplementation, they gained even stronger control of their blood glucose, insulin, and cholesterol.
Posted by DIN GTF at 8:48 PM
Add By Google:
| Foods That Cause Diabetes
Diabetes Can Be Prevented & Cured! Learn About Diabetic Foods To Avoid
www.DiabetesMellituscare.com
|
| Chromium Supplement Facts
Learn How Chromium Can Help Your Health In This Free Article.
www.LifeScript.com
|
| Chromium supplement Plus: MultiVit Rx daily formula Formulated by Ray Sahelian, M.D.
www.PhysicianFormulas.com
|
| Low protein level?
UNJURY protein supplement for low protein, protein deficiency. $18.95
www.UNJURY.com
|
| Diabetes Drinking
Diabetes and alcohol-Do they Mix? Staying safe when drinking alcohol.
|
http://www.blogcatalog.com/search.frame.php?term=gtf+chromium++Dr.Frank+Mao&id=8cadf72d8e3fec14fb03d23ce87a6c28
Wednesday, August 27, 2008
Endocrinologist Explained About GTF
Prof. Mao, Chia-Hung Frank (Dairy Specialist and Endocrinologist) successful in transferring the technology of“Glucose Tolerance Factor” to Maxluck Company.
By using lactoferrin, a kind of protein, as the carrier of trivalent chromium, the body easily absorbs the chromium and blood glucose levels are lowered
In a news dispatch from Yahoo! Taiwan News, the endocrinologist’s breakthrough was described as such.
"Let’s say the [human] cell is a house and insulin is the key [to] the house. Without chromium, which is the person using the key, the door cannot be opened and glucose cannot enter the cell.
"Once again, Professor Mao discovered that lactoferrin is the best carrier for trivalent chromium as our body can easily absorb it."
Trivalent chromium from natural foods is not easily absorbed by the body. Studies have shown that the body absorbs only up to 3% of the substance.
Chromium is a constituent ingredient of what is called the Glucose Tolerance Factor (GTF). It works closely with insulin to facilitate the uptake of glucose into cells. In individuals with impaired glucose tolerance, such as those with diabetes, hypoglycemia, and obesity, supplementation with chromium is of paramount importance. Without chromium, blood sugar levels stay elevated because the action of insulin is blocked so that glucose is not transported into the cells.
According to Dr. Mao, more than 80 percent of all diabetic cases arise from lack of GTF chromium as in the case of most Type II diabetics.
Dr. Mao also revealed that trivalent chromium in a natural form imitates the action of colostrum or a mother’s first milk. Colostrum has vast amounts of antibodies that serve as protection for the infant’s throat, lungs and intestines.
Dr. Mao combined chromium with colostrum extracts to create a product that mimics the potency of human breast milk.
The Perth scientist also made the world-first discovery that human breast milk contains stem cells is confident that within five years scientists will be harvesting them to research treatment for conditions as far-reaching as spinal injuries, diabetes and Parkinson’s disease.
“We already know how breast milk provides for the baby’s nutritional needs, but we are only just beginning to understand that it probably performs many other functions,” says Dr Cregan, a molecular biologist at The University of Western Australia.
The lactoferrin is a lycoprotein that is capable of combining with metal ions. Each lactoferrin molecule can be combined with two trivalent chromium ions.”
Laboratory tests were carried out to ensure the effectiveness of the GT&F Milk Powder produced by Dr. Mao through Maxluck Biotechnology Corporation.
The manufacturer of the product has secured approvals and endorsements from the Food and Drug Administrations of more than 20 countries, including the US, UK, France, Germany, Japan, Korea, Indonesia, Singapore, Malaysia, Taiwan and the Philippines.
See also : http://www.unhinderedliving.com/chromium.html
Posted by DIN GTF at 12:13 PM
http://www.blogcatalog.com/search.frame.php?term=gtf+chromium++Dr.Frank+Mao&id=078d79765707ce61cd22a36b3893dfbd
Saturday, January 17, 2009
LACTOFERRIN, CHROMFERRIN AND GTF-Chromium Supplement
Lactoferrin : Multifunctional Health Food
GT&F is a good GTF-Chromium supplement. Professor Frank Mao used a breakthrough patented technology to combine chromium with lactoferrin to form a lectoferrin-chromium complex known as Chromferrin.
This invention is due to the discovery by Professor Frank Mao, GTF-Chromium is readily and easily absorbed into our body by using lactoferrin as carrier, hence prevents chromium deficiency in our body.
What is Lactoferrin?
Lactoferrin is minor protein found naturally in the milk of most mammals including human and cow.
It is part of the transferrin family, meaning that it has the ability to bind strongly whith iron also transport iron.
How Lactoferrin Works?
Lactoferrin is often referred to as a innate defense protein and a frequent first-line-of-defense in protection against pathogens.
It maintains immunomodulatory properties to aid the immune system, provides a natural ability for deference against bacterial, fungal and viral pathogens.
Lactoferrin ensures not only the higher absorption of chromium into our body easily. Researches also show that lactoferrin could also play a role in controlling diseases including:
a. various type of cancers
b. lung infections
c. gastointestinal disorders
d. diseases caused by inflammation
e. diabetes
Researches have shown Lactoferrin to have the following functions:
Posted by DIN GTF at 9:42 AM
http://www.blogcatalog.com/search.frame.php?term=gtf+chromium++Dr.Frank+Mao&id=0317665b69400f1d285feb25fe3088e2
Monday, June 30, 2008
Chromium supplements may help diabetics
Mon, 10 Mar 2008
The usual treatment and management of diabetes is carried out with medication and lifestyle changes in addition to supplements, a popular one being ampalaya (bitter melon). Another supplement to have a good effect on diabetes is chromium but in particular trivalent chromium.
The human body needs chromium, a trace mineral, to help the body grow properly stay healthy and helps burn carbohydrates and fats . Chromium bases research has been ongoing for the past 50 years. Many of the studies showed that chromium supplements helped diabetics and other animals to restore control of blood sugar .
One of the researchers is Taiwanese dairy specialist and endocrinologist Dr Frank Mao Chia Hung of Maxluck Biotechnology Corp. and the Taiwan Chung Hsing University, who worked on the theory that most types of diabetes is a result of a deficiency of GTF in the body.
Khoo Boo Boon, president and CEO of GTF Worldwide Philippines said, "The GTFs most important component is trivalent chromium and Mao found that when its levels are low, human cells are unable to absorb glucose properly, resulting to hyperglycemia or high blood sugar."
Khoo added the supplement is essential as trivalent chromium cannot easily be absorbed by the body. Other researchers have verified Mao’s findings. A clinical trial in four Taiwan hospitals showed that the control group of diabetics who drank GT&F milk powder had lower amounts of fasting plasma glucose so reducing their need for insulin injections and other medicines.
Source : diabeticlife.co.uk
Recent Testimonial, Mr Kubik, Australian, wrote:
I feel very good. yesterday I had 6.5! However, when I've tried eat some carbs, my BG went to 9.4!
So with strict diet and every day 30 minutes walk plus Diabex plus GT&F, plus Gimnema Silvestri
I can maintain at this stage regular 6.5-7.00
IMHO it's not revolutionary result, but is definitely helping a lot.
Maybe it's not very important but... I've noticed that I need less sleep. Usually I was sleeping 6-7 hours per night, lately
I sleep 5.5 - 6 hour per night and I have a lot of energy!
Date : Jun 30, 2008
Posted by DIN GTF at 8:58 AM
Profile of Dr.Waiter Merz.
He discovered GTF 1970th.
http://www.patentstorm.us/patents/4918102/fulltext.html
http://www.patentstorm.us/patents/5013752/fulltext.html
2. Description of Prior Art
Dr. Walter Merz of the Human Nutrition Laboratory in Bethesda, Md., was the first scientist to describe the occurrence and function of chromium in biological systems (Physiological Rev. 49:163, 1969). This was followed in 1970 by the proclamation of Dr. Henry A. Schroeder, Professor of Physiology Emeritus at the Darmouth Medical School, that chromium deficiency was a factor in atherosclerosis (Jour. Chronic Diseases 23:123). Regrettably, this knowledge was not then recognized, accepted, and applied to medical practice. Most recently, Gary W. Evans, PhD, and Muriel B. Gilman at Bemidji State University, Mont. 56601, have prepared a paper (for 1989 publication in one of the journals of the American Chemical Society) titled "Anabolic Effect of Chromium Picolinate". Therein they identify metabolic mechanisms showing how ingestion of naturally occurring chromium beneficially decreases LD ("bad") cholesterol and increases HD ("good") cholesterol in blood serum. They link these observations to "death from heart disease" and to treatment and prevention of diabetes.
Linda Chian is Dr.Mao's supporter and together formed
company Maxluck Biotechnology Corp. to bring to the world their common belief that biotechnology breakthrough in nutritional supplements offer big technological opportunity to improve people's lives and the environment.
Core Team
The members of the core team are responsible in bringing the much-applauded and patented biotechnology GT&F NutriPack, GT&F NutriCap and GT&F NutriCare-Kids products to the Philippines. The ties binding them together is their common belief that biotechnology breakthrough in nutritional supplements offer big technological opportunity to improve people's lives and the environment.
PROF. FRANK MAO CHIA HUNG, Dairy Scientist and Endocrinologist Extraordinaire
Prof. Mao is the inventor of the widely patented GT&F Lactoferrin-chromium Glucose Tolerance Factor (GTF) Nutripack and Nutricare-Kids. This learned professor, who is currently the director of Taiwan Chung Hsing University, is a dairy specialist as well as an endocrinologist by training . He earned his Msc and PhD in Endocrinology from the University of Wisconsin, Madison, in the United States and spent years researching on diabetes and metabolic syndrome.
For Dr. Mao, hyperglycemia (high blood glucose) is a symptom rather than a disease. Thus, the key issue in the treatment of high blood glucose is addressing the hindrance that prevents glucose from entering cells. The real focus according to him, should be enhancing the bioactivity of insulin and the sensitivity of insulin receptors.
Working on the pioneer work of the late Dr. Walter Mertz, the discoverer of Glucose Tolerance Factor (GTF) - a complex compound of trivalent chromium, essential amino acids and other trace elements that play an important role in human metabolism, Prof. Mao employs patented biotechnology processes in creating a natural form of GTF which mimics human colostrums. The significance of his discovery lies in the fact that: 1) trivalent chromium in the body declines with age, obesity, pregnancy, alcohol abuse, pollution, stress, etc., 2) chromium commonly found in vegetables and nuts and other synthetic form is not easily absorbed in the human body. Depletion of chromium in the body will affect metabolism and lead to diseases.
A randomized-controlled clinical trial of the beneficial effect of GT&F milk powder on diabetes was published in the renowned medical journal Metabolism in July 2006 (55:923-927). In addition, his pioneer work and patented biotechnology success was cited as early as year 2001 in the New Zealand Herald (4th July 2001) in a featured article on biotechnology research titled "Our Turn: Science meets morals in the next great leap" by Simon Collins.
MADAM LINDA CHIANG CHENG LIN-HUI, Chairman of Maxluck Biotechnology Corp.
Madam Linda Chiang is known all over Taiwan as the "Mother of Biotechnology in Taiwan" for her relentless pursuit of innovation through Biotechnology and bionanotechnology research to benefit humanity. She is also the prime mover of the industry-academe cooperation that is recognized today as one of the most successful models of biotechnology in Taiwan. It is through her initiative that Maxluck Biotechnology Corporation began as a company at the National Chung Hsing University Incubator Facility, undertaking research and development on Glucose Tolerance Factor and insulin metabolism which resulted in the discovery of GT&F Blended Milk Powder and Capsules. For her numerous contributions to society and humanity particularly her dedication to biotechnology research, Madam Linda Chiang was bestowed the First National Chung Hsing University (NCHU) World distinguished Alumni Award.
http://www.mygtfworld.com/index.php/main/advisor
GT&F FOR VITALITY
After the discovery of the health benefits of GTF chromium, thousands of scientific researches have been carried out to produce chromium products. However, the effectiveness of the products is not encouraging, as most products found in the market are either of low absorption rates or are in an unstable form. It is important to note that in order to be best absorbed and fully utilized, chromium should exist in the form of GTF. In the GTF molecule, chromium is in its organic form. The trivalent chromium combines with nicotinic acid or B3 and other amino acids which are glycine, cysteine, glutamic acid.
GTF is a superior product formulated and produced under painstaking researches by a group of scientists in Taiwan led by Dr. Frank Mao Jia-Hung. It is the only form of chromium that is biologically active with lactoferrin as its carrier. It is in its most natural form and it emulates human breast milk; therefore it is highly effective and potent. In fact, two randomized, double-blind, placebo-controlled trials have proven the potency of GT&F in improving metabolism.
CONCLUSION
Indeed, there is no single panacea for raising energy levels and making one feel great. While there are a lot of energy products in the market, one
should choose the product that can best address the underlying health problems concerning low energy levels. From the review of scientific facts in this paper, it is GTF chromium that makes the difference. Therefore, besides healthy balanced diet, regular exercise, good quality of sleep and so forth, GT&F supplement should be included in one's road map to smart and energetic life.
REFERENCES
[1] McLead MN & Golden RN (2000) Chromium treatment of depression, international journal of Neuropsychopharmacology 3: 311-4, cited in Jamison JR (2003) Clinical guide to nutrition & dietary supplements in disease management, pg 257 Chrurchill Livingstone.
Click here for he GTF Web Site
http://www.mygtfworld.com/main/management_team.html
Click here for News Articles on the GTF Web Site
http://www.mygtfworld.com/main/newsarticles.html
Click here to access a copy of Diabeties
a journal produced by the American Diabeties Association
With an Impact Factor of 8.3, Diabetes is the highest-ranked journal devoted to original research in diabetes
World Diabetes Day
is celebrated each year on November 14. It is a global awareness campaign run by the International Diabetes Federation. Help us to increase diabetes awareness - www.worlddiabetesday.org
http://www.worlddiabetesday.org/
World Diabetes Day is an official United Nation’s World Health Day. It is celebrated every year on November 14. The date was chosen because it marks the birthday of Frederick Banting, who, along with Charles Best, is credited with the discovery of insulin in 1921. World Diabetes Day is represented by a blue circle logo. The blue circle is the global symbol of diabetes and signifies the unity of the global diabetes community in response to the diabetes pandemic.
World Diabetes Day was created by the International Diabetes Federation (IDF) and the World Health Organization (WHO) in 1991, in response to concern over the escalating incidence of diabetes around the world. The International Diabetes Federation leads the World Diabetes Day campaign – produces the annual and biannual themes, runs the global website, creates all the materials and drives the global outreach.
The theme for 2009-13 is Education and Prevention. Recent themes were Diabetes and Obesity (2004), Diabetes and Foot Care (2005), Diabetes in the Disadvantaged and the Vulnerable (2006) and Diabetes in Children and Adolescents(2007-2008).
Through its Unite for Diabetes campaign, IDF led the push for a UN Resolution on diabetes. On December 20, 2006, that goal was realized when the United Nations General Assembly unanimously passed Resolution 61/225, which designates the existing World Diabetes Day as a United Nations world day, to be observed every year beginning in 2007.
World Diabetes Day is a global event. It brings together millions of people in over 160 countries to raise awareness of diabetes, including children and adults affected by diabetes, healthcare professionals, healthcare decision-makers and the media. Numerous local and national events are organized by the member associations of the International Diabetes Federation and by other associations and organizations, healthcare professionals, healthcare authorities, and individuals with an interest in diabetes. World Diabetes Day unites the global diabetes community to produce a powerful voice for diabetes awareness.
Diabetes organizations and individuals worldwide establish a range of activities tailored to a variety of target audiences. Activities organized every year include such things as: lighting of global monuments, buildings and individual homes in blue on November 14, formation of blue circles around the world, global diabetes walks and rides, a WDD car in the Baja 1000 race, WDD motorcycle, press conferences, in-school activities, sports activities, frisbee events, free screenings for diabetes and its complications, workshops and exhibitions, and geocaching.
Click here for more information on World Diabetes Day on FaceBook-Japan Click to access Japanese Diabetes.net
http://app4.websitetonight.com/WST.aspx
Click here to acces the Japan Diabetes SocietyJapan Diabetes Society
Diabetes.co.uk your one stop resource for diabetes, diabetics, diabetes researc, diabeteseducation and advocacy for people with diabetes, ...
http://www.diabetes.co.uk/
-
What's New on Diabetes.co.uk
This is where you'll find the latest additions to Diabetes.co.uk, the global diabetes community.
Latest Guides & Site Features
- Diabetes charities - updated/added 30 March 2009. List of diabetes charities with profiles, information, links and ability to donate online to some of the charities.
- Healthcare professionals - information regarding GPs, PCTs, DSNs and more. Added 2 Feb 2009.
- Diabetes types - information on the different diabetes types - added 21 Jan 2009.
- Type 3 diabetes - information about a possible third diabetes type identified by US scientists - added 21 Jan 2009.
- List of Diabetes Jargon (compiled by the Diabetes Support Forum) - added 9 Jan 2009.
- Diabetes support forums - information about diabetes forums & how they can be used. Added 4 Dec 2008.
- Diabetes help and support - if you're new to Diabetes.co.uk, start here. Added 2 Oct 2008.
- Blood sugar converter - calculate from mmol/L to mgl/dl and vice versa.
- Byetta - information on Byetta. Added 13th June 2008
- Januvia - guide to Januvia. Added 13th June 2008
- Diabetic Foot Ulcers - information on foot complications and ulcers. Added 13 June 2008.
- Diabetic Nerve pain - information on nerve pains associated with diabetes. Added 13 June 2008.
- Free Bayer Blood Glucose Meters - choose whether you'd like a Contour or Breeze 2.
- Diabetes Events - see upcoming events and add your own. Added: 23rd May 2008.
- Diabetes Petitions - respond to petitions, read the response or create your own petition or campaign. Added: 23rd May 2008.
- Diabetes and Metformin - added 29th April 2008
- Diabetes and Metformin FAQs - added 29th April 2008
- Diabetes and Sport - added 25th March 2008
- Sport Tips for Diabetics - added 25th March 2008
- Diabetes & Extreme Sports - added 25th March 2008
- Diabetes, Sport and Blood Glucose - added 25th March 2008
- What is Diabetes - updated 25th March 2008 (with an overview, symptoms and control information)
- Diabetes UK Careline - service provided by Diabetes.org.uk (19 February 2008)
- Updated: Type 2 diabetes (7 February 2008)
- Updated: Blood glucose meters (7 February 2008)
- Sleep Apnea and Diabetes - information on sleep apnea
- Diabetes Screening Test - information about diabetes screning tests
- Diabetes Screening Test FAQ's - popular questions regarding screening tests
Competitions
- Take That competition - win 2 Take That tickets for their Conventry gig
General
- Diabetes book reviews - 2 new book reviews
- Diabetes Forum - the diabetes forum has been rejuvenated for the new look site
- Free Competitions - we've got a whole feast of competitions for the first month of 2008
- Diabetes guides - find the information you're looking for with our diabetes guides
Insulin & Medication
- Insulin prescription - aims to answer insulin prescription questions
- Insulin side effects - about the side effects of insulin
- Insulin overdosage - how to spot an overdose, and what to do in the situation
- Diabetes lancets and lancing - information about lancing
- Diabetes lancing devices - the types of lancing devices available
- Insulin pumps - information about insulin pumps
- Wearing and using an insulin pump - how to wear and use insulin pumps
- Getting an insulin pump - how to obtain insulin pumps
Diabetes.co.uk Site Features
Home- Diabetes Directory
- Diabetes News
- Global Diabetes
- UK Diabetes Industry
- Diabetes Cure
- Diabetes Signs & Symptoms
- Diabetes Guides
- Diabetes Support Forums
- Diabetes Toolbox
-
Diabetes Care
Blood Sugar Converter- Blood Readings to Plasma Readings Converter
- BMI Calculator
- HbA1c to Blood Sugar Level Converter
- Initiation Insulin Dose Calculator
- Weight & Volume Converter
-
Diabetes Media
-
NHS and Diabetes
-
NHS is the National Health Service in the United Kingdom
Diabetes in the UK is often treated entirely by the National Health
Service. The NHS provides structured care for people with diabetes of every type and at every stage.
Diabetes is a complex condition and therefore NHS diabetes care must be similarly complex. Many people with diabetes are not aware of NHS diabetes care services, initiatives in their area, and the support available.
This section has been created to provide a central platform for our visitors to browse NHS diabetes services, locally and nationally.
The NHS faces serious difficulties in dealing with diabetes care, from pre-diabetes to blood glucosemanagement to trying to avoid the complications of diabetes. With millions of people with diabetes in the UK, diabetes places a great strain on NHS resources.
NHS diabetes spending
Estimates indicate that the NHS spends some 9% of total hospital expenditure on treating diabetes and diabetes complications. Furthermore, an estimated 10% of NHS hospital beds are occupied by people with diabetes. A report entitled 'Diabetes in the NHS' estimated a total cost of £3.5 billion per annum, over £9.6 million each day.
With over 100,000 people with diabetes being diagnosed each year, it is easy to see how these health costs could spiral.
How does the NHS deal with diabetes?
Most NHS diabetes care is handled by multidisciplinary teams. The NHS has brought diabetes care closer to home and started to involve technology in handling diabetes. As well as a consultant diabetologist, an NHS team may include Diabetes Specialist Nurses, dietitians and podiatrists.
-
Caring for Diabetes
Many of those with diabetes are unsure as to how to care for their condition. There is often confusion surrounding blood glucose and how to monitor it correctly. Some diabetics are also unaware of the sweeteners they can use instead of sugar.
This area of Diabetes.co.uk has been developed to understand the options available:
- Blood glucose monitor guide
- Blood glucose monitors and data management
- Diabetes and blood glucose
- Diabetes and low calories sweeteners
- Diabetes blood glucose and blood sampling
- Diabetes test strips
- Blood sugar converter - useful for converting from mmol/L (UK) to mg/dl (US) and vice versa
- The importance of coding - no coding meters, information and availability
- Diabetes and stress
You may also be interested in our Diabetes Recipes archive.
Pre-Diabetes
Pre diabetes is an enormous and blossoming problem, closely tied to obesity. If strong preventative and educational steps are not taken by all nations, immediately, then the future burden on healthcare will be enormous.
What is pre-diabetes?
Pre-diabetes is almost always a precursor to the development of type 2 diabetes. It is characterised by the presence of higher than normal blood glucose levels that are yet to reach diabetic levels. The scale of the problem is enormous and growing, as Western society and diet becomes more pervasive. In the United States alone there are over 40 million people suffering from the pre-diabetic condition.
Diabetes and Blood Glucose
-
Blood glucose and blood sugar are interchangeable terms, and both are crucial to the health of the body. Most diabetics will be familiar with the terms blood glucose, blood glucose test, blood glucose level and blood glucose meter, but what does blood glucose really mean? Why do blood sugar levels need to be controlled?
What are blood glucose levels?
Blood sugar levels are literally the amount of glucose in the blood, sometimes called the serum glucose level. Usually, this amount is expressed as millimoles per litre (mmol/l) and stay stable amongst non-diabetic people at around 4-8mmol/l. Spikes in blood sugar will occur following meals, and levels will usually be at their lowest in the early mornings. When it comes to diabetics, blood sugar fluctuates more widely.
-
Why do blood glucose levels need to be controlled?
High levels of glucose present in the blood over a sustained period of time end up damaging the blood vessels. Although this does not sound too serious, the list of resultant complications is. Poorly controlled blood glucose levels can increase your chances of developing diabetes complications including nephropathy, neuropathy, retinopathy and cardiovascular diseases. The time-scale for the development of these complications is usually years, but be aware that type 2 diabetes is often not diagnosed until a relatively late stage. -
How do I find out what my blood glucose levels are?
-
You can use home testing kits, although before doing so read our guide to blood glucose monitors. Measure levels by putting a drop of blood on a strip and placing it into the BGM (blood glucose meter.) Prick your finger with a specially designed lancet to draw blood.
-
What is a good blood glucose level?
A normal pre-prandial (before meal) blood glucose level will be between 4 and 7 mmol/l. After eating (post-prandial) levels should be less than 10 mmol/l when tested 90 minutes after a meal. When going to bed for the night, levels should be about 8mmol/l.
When should blood glucose levels be measured?
The number of times per day blood glucose levels should be measured depends entirely on the diabetics. Type 1 diabetics using insulin should check their blood sugar levels before every meal, sometimes as often as five times per day. For type 2 diabetics controlling their condition with diet, you should test several times a week. However, this doesn't apply to everyone, and each individual case should seek expert advice.
Are there special times when blood glucose should be measured?
Any time you feel ill, and over time if you can feel your blood sugar becoming too low or too high, you should check your blood glucose levels. You should also be aware that a reading over 20mmol/l should prompt a urine test for the presence of ketones.
What is an HbA1c test and how does it relate to blood glucose?
HbA1c tests show average blood glucose levels over a sustained period of time. HbA1c is glycated haemoglobin and more of it is produced in the body by high blood glucose levels. Different scores of HbA1c show good, fair, poor and bad control of diabetes. Increasing HbA1c levels indicate greater risk of complications.
What is a good blood glucose level?
A normal pre-prandial (before meal) blood glucose level will be between 4 and 7 mmol/l. After eating (post-prandial) levels should be less than 10 mmol/l when tested 90 minutes after a meal. When going to bed for the night, levels should be about 8mmol/l.
When should blood glucose levels be measured?
The number of times per day blood glucose levels should be measured depends entirely on the diabetics. Type 1 diabetics using insulin should check their blood sugar levels before every meal, sometimes as often as five times per day. For type 2 diabetics controlling their condition with diet, you should test several times a week. However, this doesn't apply to everyone, and each individual case should seek expert advice.
Are there special times when blood glucose should be measured?
Any time you feel ill, and over time if you can feel your blood sugar becoming too low or too high, you should check your blood glucose levels. You should also be aware that a reading over 20mmol/l should prompt a urine test for the presence of ketones.
What is an HbA1c test and how does it relate to blood glucose?
HbA1c tests show average blood glucose levels over a sustained period of time. HbA1c is glycated haemoglobin and more of it is produced in the body by high blood glucose levels. Different scores of HbA1c show good, fair, poor and bad control of diabetes. Increasing HbA1c levels indicate greater risk of complications.
What is a good blood glucose level?
A normal pre-prandial (before meal) blood glucose level will be between 4 and 7 mmol/l. After eating (post-prandial) levels should be less than 10 mmol/l when tested 90 minutes after a meal. When going to bed for the night, levels should be about 8mmol/l.
When should blood glucose levels be measured?
The number of times per day blood glucose levels should be measured depends entirely on the diabetics. Type 1 diabetics using insulin should check their blood sugar levels before every meal, sometimes as often as five times per day. For type 2 diabetics controlling their condition with diet, you should test several times a week. However, this doesn't apply to everyone, and each individual case should seek expert advice.
Are there special times when blood glucose should be measured?
Any time you feel ill, and over time if you can feel your blood sugar becoming too low or too high, you should check your blood glucose levels. You should also be aware that a reading over 20mmol/l should prompt a urine test for the presence of ketones.
What is an HbA1c test and how does it relate to blood glucose?
HbA1c tests show average blood glucose levels over a sustained period of time. HbA1c is glycated haemoglobin and more of it is produced in the body by high blood glucose levels. Different scores of HbA1c show good, fair, poor and bad control of diabetes. Increasing HbA1c levels indicate greater risk of complications.
-
What is a good blood glucose level?
A normal pre-prandial (before meal) blood glucose level will be between 4 and 7 mmol/l. After eating (post-prandial) levels should be less than 10 mmol/l when tested 90 minutes after a meal. When going to bed for the night, levels should be about 8mmol/l.
-
NHS Milton Keynes
-
NHS Milton Keynes has launched a brand new section to their website, dedicated to diabetes.
What is the aim of the new section?
The aim of the new site, MiltonKeynes.nhs.uk, is to guide people towards relevant information and support services, depending on their circumstances.
The section caters towards people who are worried that they may have diabetes, those who have just been diagnosed, and those who are living with diabetes.
The personalised information provided aims to:
- Inform people about diabetes.
- Help people find answers to the questions they may have about diabetes.
- Help people to manage their diabetes or reduce their risk of getting the condition.
- Provide relevant video interviews of people talking about their experiences of living with diabetes
- Direct people towards reliable online information available.
- Inform and guide people towards the many local services in Milton Keynes .
Why the new section?
NHS Milton Keynes hopes that the section will help people to access quickly all the information they require about diabetes, as well as guide them towards the comprehensive range of services available in the Milton Keynes area.
The support services available in the Milton Keynes area include specialist help in managing diabetes, dietary advice groups, fun-led support for children with diabetes and services for more specific diabetes-related concerns such as podiatry services and services to help quit smoking.
The section will help to direct people to such services, as well as to the wealth of information and support available on the website. In this way, the site hopes to make it easier for people with diabetes to access reliable information and support, so that they can get on with living a normal, healthy lifestyle to the full
-
Diabetes and Life
-
http://www.diabetes.co.uk/whats-new-on-the-site.html
- Diabetes & Travel
- Diabetes & the Pill
- Driving with Diabetes
- Diabetes Emergencies
- Diabetes & Sex
- Diabetes Employment
- Diabetes & Smoking
- Diabetes & Depression
- Diabetes & the Elderly
- Diabetes & Dentistry
- Diabetes History
- Fake Diabetes Cures
- Diabetes Charities
- Diabetes and Diabulimia
- Diabetes and Saving Money
- Diabetes and Children
- http://www.diabetes.co.uk/whats-new-on-the-site.html
Diabetes Complications
http://www.diabetes.co.uk/whats-new-on-the-site.html
- Diabetes Complications
- Diabetes & Footcare
- Diabetes & Erectile Dysfunction
- Diabetes & Coeliac
- Diabetes & Ketones
- Diabetes & Amputation
- Diabetes & Nocturia
- Diabetes & Cholesterol
- Diabetes & Foot Ulcers
- Diabetes & Nerve Pain
Diabetes Diet & Fitness
http://www.diabetes.co.uk/whats-new-on-the-site.html
- Diabetes Recipes
- Subscribe Recipe
- Diabetes Food Forum
- Alcohol Substitutes
- Diabetes Cooking
- Diabetes Diet Basics
- Diabetes Nutrition
- Diabetes & Weight Loss
- Diabetic Exchange
- Diabetic Exchange FAQ
- Meal Planning
- Recipe Archive
- Vegetarian Diet
- Tools/Calculators
Diabetes, Sport and Exercise
http://www.diabetes.co.uk/whats-new-on-the-site.html
- Diabetes and Fitness
- Exercise and Diabetes
- Diabetes and Sport
- Sport Tips for Diabetics
- Diabetes & Extreme Sports
- Diabetes, Sport and Blood Glucose
- General Information available on Diabetes.co.uk site
- http://www.diabetes.co.uk/whats-new-on-the-site.html
Diabetes TypePre-DiabetesMedication & Insulin
-
Diabetes.co.jp - A Lilly Diabetes Resource
https://www.diabetes.co.jp/ - 37k -
Diabetes develops due to a diminished production of insulin (in type 1) or resistance to its effects (in type 2 and gestational). Both lead to hyperglycemia, which largely causes the acute signs of diabetes: excessive urine production, ... en.wikipedia.org/wiki/Diabetes
-
Changing Diabetes
Changing Diabetes
www.novonordisk.co.jp/documents/article_page/document/changingdiabetes.
- [PDF]
Diabetes
PDF/Adobe Acrobat - HTML
1. Diabetes. Diabetes is a disease in which your body cannot properly use the food you eat for energy. Your cells need energy to live and grow. When you eat, food breaks down into a form of energy called glucose. Glucose ...
www.healthinfotranslations.com/pdfDocs/diabetes-JP.pdf - - [PDF]
Diabetes During Pregnancy
PDF/Adobe Acrobat - HTML
Diabetes During Pregnancy. If you have diabetes, your body cannot properly use the food you eat for energy. When you have diabetes during pregnancy, it is called gestationaldiabetes. When you eat, your body breaks down the foods into a ...
www.healthinfotranslations.com/pdfDocs/diabetes-pregnancy-JP.pdf - -
TEAM DIABETES JAPAN -Team Diabetes Japan
No Limit
www.nittokyo.or.jp/teamdiabetes_10001.html - 18k -
????
Diabetes Book Reviews
http://www.diabetes.co.uk/Diabetes-Book-Reviews.html There are a number of diabetes books on the market, and choosing the right one will depend on how long you have been diagnosed for, what you need to know about, and how much you are willing to spend. Books for diabetes include diabetes diet books, diabetes cook books/diabetes recipe books, and diabetes reference books. A number of niche diabetes books also exist, including diabetes books for children and books about diabetic complications. This section of Diabetes.co.uk provides a range of book reviews to help you in your diabetes book choices. Book reviews are added on a monthly basis.
Getting diabetes diet right is one of the most difficult parts of having the disease. In recent years, expert consensus about the best food for diabetics to eat has shifted. Nowadays, the experts say, we can eat anything (or nearly anything), but a good diet makes all the difference to blood glucose control.
Read review | Buy the book
The days, weeks and months following diagnosis can be a perplexing and arduous period. The key to early treatment of diabetes is information - knowing the intricacies of the disease and even more importantly your own responses and idiosyncrasies.
Read review | Buy the book
The media is full of diabetes books and diabetes treatments that claim to 'cure' diabetes. This usually amounts to a hollow promise at best, or a cynical marketing ploy at worst. Conventional medical lore dictates that type 2 diabetes is irreversible.
Read review | Buy the book
Teenage Diabetes and Blood Glucose Testing Taking control of diabetes and establishing an effective routine is the key to cutting down the risk of diabetic complications. Controlling your blood glucose levels automatically means a decrease in the risk of developing diabetes complications. Keeping levels at the average level for as long as possible is the key. Pre-prandial (before meals) readings should stand between 4-6mmmol/l, whilst post-prandial (two hours following a meal) readings should be 10mmmol/l. These figures are intended as a basic guide rather than numbers to be strictly adhered to. Unfortunately for diabetic young people, and those who are newly diagnosed, tests can be confusing without being dangerous. Tests can sometimes yield a surprisingly high or low result, and although these should always be treated with caution, a single high or low result is not always a cause for panic. Instead, diabetes experts advise keeping an even closer eye than usual on your blood glucose levels. Wherever you are and whatever you are doing, keeping your testing regular allows you to have the greatest level of control over your diabetes possible. This can seem, literally, painful. Having to interrupt a busy day, or a fun occasion, just to test the blood can be easy to ignore, especially when the results seem to be similar all the time anyway. There is nothing wrong with being confident when it comes to testing for diabetes, but thinking that you can feel your blood glucose levels is not always entirely accurate. Diabetes experts advise teenagers to keep a close monitor using test strips and a meter. Particularly important testing times include early in the morning, before and after physical activity (of whatever type), before and after meals, and if you feel unwell at any time. As a diabetic teenager, your healthcare team should have shown you how to use a blood glucose meter. When you test your blood using a meter, the result will display how much glucose is in your blood. The meter reads off your results by combining your blood (by pricking your finger) with a test strip. Meters and test strips from a reputed provider are completely accurate, providing the equipment is properly looked after and test is correctly carried out. Looking after diabetes testing kit is essential, and if you feel that your kit is in any way damaged or inaccurate it should be replaced immediately. Exposing a blood glucose meter or testing strips to direct sunlight or intense cold is also a bad idea.
http://www.diabetes.co.uk/Teenage-diabetes-and-blood-glucose-testing.html
A busy social life, sports and work at school, blossoming relationships and dealing with your parents are all things that teenagers have to cope with. Having diabetes on top can make things more difficult, and regular diabetes testing is the key to keep the risk of developing complications down and the energy levels up.
Avoiding diabetes complications as a teenager using regular testing
What should I do if my blood sugar climbs above 10mmmol/l?
Regular diabetes testing as a teenager
What does a blood glucose monitor do?
Looking after diabetes testing kit
Diabetes Shop: Test Strips
Find out more about diabets products and equipment and buy in line
http://www.diabetes.co.uk/Teenage-diabetes-and-blood-glucose-testing.html
Convert HbA1c to Average Blood Sugar Level
http://www.diabetes.co.uk/hba1c-to-blood-sugar-level-converter.html
Use this calculator to convert HbA1c to Average Blood Sugar Level.
The HbA1c level in your blood indicates what your average blood glucose level has been in the past 4 weeks, approximately.
Everyone, whether non-diabetes, pre-diabetic, type 1 diabetic or type 2 diabetic has some degree of sugar in their blood.
Amongst people who do not have diabetes, normal sugar levels in the blood range from approximately 70mg/dl to 120 mg/dl. When people eat, their blood sugar level increases, but returns to normal quickly, usually after one or two hours.
To convert between mg/dl and mmol/L, use our blood sugar converter.
For people with diabetes, keeping blood sugar in the 70mg/dL – 150 mg/dL range is considered safe before a meal. Around two hours after a meal, people with diabetes should aim to have under 200 mg/dL in their blood.
More Information
Blood Sugar Converter
http://www.diabetes.co.uk/blood-sugar-converter.html
Convert blood sugar/glucose from mmol/L (UK standard) to mg/dl (US standard) and vice versa using our blood sugar converter.
Whats the difference bettwen mmol/L and mg/dl
Both are used to measure blood sugar levels. The only difference is the country in which they are most commonly used. mmol/L is the most common measurement used in the UK with mg/dl predominantly used in the USA.
- mmol/L: Millimoles per litre
- mg/dl: Milligrams per 100 millilitres
Blood glucose typically varies from 4.5 mmol/L to 6 mmol/L for people without diabetes.
Blood sugar (also called blood glucose) is tightly controlled in the human body. Measuring blood sugar levels and understanding what your glucose levels should be is an essential part of diabetes treatment for many people with diabetes. Blood sugar level refers to the total amount of glucose circulating in the blood. In different parts of the world, different units for measuring blood glucose are standard. Diabetes.co.uk has developed this useful tool to help you convert blood glucose units quickly and easily.
Guide to Blood Glucose Meters (Blood Glucose Monitors)http://www.diabetes.co.uk/diabetes_care/blood_glucose_monitor_guide.html
Keeping an accurate idea of your blood glucose levels is an integral part of successful diabetes management. Blood glucose meters are one piece of diabetes-related technology that simplifies everyday diabetes treatment. Urine testing remains important (particularly to check for the presence of ketones ), but having an accurate blood sugar meter makes sense for staying on top of your disease.
Choosing the right meter will depend on the products available to you, the cost of test strips (or NHS prescription availability) and the most suitable device for your individual requirements. You should discuss your options with your healthcare team and GP before purchasing, and always make sure to compare prices. Some people prefer to have more than one blood glucose monitor - one for home and one for the office, or one for home and one for travelling.
Your healthcare team should be able to advise on how many times per day you need to check your blood sugar levels.
How easy are blood glucose meters to use?
This will depend on the design interface favoured by the manufacturer, but some blood glucose monitors are definitely easier to use than others. For instance, some meters require a smaller drop of blood to give a reading. Investigate the process before purchasing and speak to as many peers and experts as possible.
How accurate are blood glucose meters?
All meters on the market should have a high degree of accuracy. Because of the possible implications if they are inaccurate, most manufacturers make certain that their products give accurate readings. However, testing the meter regularly to ensure that it is still accurate is a good idea, as meters can become less accurate over time.
How do I test the accuracy of my blood glucose meter?
Many professionals recommend checking the accuracy of your blood glucose meter at least once every month. The best way to do this is to use the meter at the same time you visit the doctor for a test, and then compare the two results.
Why might a blood glucose meter become inaccurate?
Blood glucose meters may malfunction and become inaccurate should they be dirty, ageing or if they become too hot or damp. Furthermore, if the strips are outdated or the meter has a problem calibrating with the strips, the meter may malfunction. Meters should be cleaned regularly, and taken care of like any other electronic device.
Are blood glucose meters portable?
All blood glucose meters today are light to carry and are mostly run on batteries, meaning that portability is not usually an issue. When it comes to carrying your meter on board a flight, you should prepare by getting a letter from your GP in advance.
How long do tests take using blood glucose meters?
Most meters don't take more than a minute to provide accurate blood sugar level results. For most people and in the case of most meters, speed of testing will not really be an issue. Many of the later model blood glucose meters will provide results in as little as five seconds.
Are meters available for people who have problems with retinopathy or other eye disorders?
Several leading brands also make audible blood glucose monitors that give verbal instructions and verbal test results to their user. This range includes meters that can speak in other languages besides English.
Pharmacy Products related to Diabetes Blood Glucose Monitors
- Accu-Chek Aviva Blood Glucose Meter
- Accu-Chek Compact Plus Blood Glucose Meter
- One Touch UltraEasy Silver
- One Touch UltraEasy Green
- One Touch UltraEasy Pink
- One Touch UltraEasy Black
- One Touch Ultra Smart System
- One Touch Ultra2 Glucose Meter
- Pasante Healthcare Blood Glucose Level Test
- Pasante Healthcare Urine Infection Test
- A+D Digital Blood Pressure Monitor UA-767
- Omron MX2 Blood Pressure Monitor
- Novofine 30g 8
- Penfine Universal Click Pen Needles 12mm
- Penfine Universal Click 6mm
- Unilet ComforTouch Ultra Thin Lancets
- Unilet ComforTouch Ultra Thin Lancets x 200
- Unilet GP Lancets
- Unifine Pentips 12mm Original
- Unilet Superlite Lancets
- Unilet Superlite Lancets x 20
http://www.diabetes.co.uk/diabetes-and-ketones.html
The presence of ketones in the bloodstream is a common complication of diabetes, which if left untreated can lead to ketoacidosis.
This section of Diabetes.co.uk is intended as an information resource for diabetes sufferers who want to know more about ketones and diabetes. If you are looking for medical advice, think you may have ketones, or would like ketone testing please contact your GP or diabetes healthcare team as soon as possible.
What exactly are ketones, and what do they have to do with diabetes?
Ketones are an acid remaining when the body burns its own fat. When the body cannot get enough glucose from the blood to use as energy (in the case of type 2 diabetics it may receive very little glucose, in type 1 cases it will receive none), it will begin to burn fat. When the body is burning too much fat, it may cause ketones to become present in the bloodstream.
2.5 million people with diabetes in the UK
Mon, 20 Oct 2008
According to the latest figures from Diabetes UK, the diabetic population of the UK has soared by some 167,000 in the last year. The total, according to the report, now stands are just under 2.5 million.
In England alone, this 6.4 per cent increase has resulted in the population crossing the two million mark for the first time. The vast majority of people with diabetes in the UK have type 2, often associated with obesity . Estimates put the obesepopulation of the UK at around 5 million.
The chief executive of Diabetes UK, Douglas Smallwood, reportedly commented: "These are truly alarming figures. Part of why we have seen such a huge increase can be attributed to improved screening from healthcare services and greater awareness amongst those at high risk oftype 2 diabetes . However, there is no getting away from the fact that this large increase is linked to the obesity crisis ."
The answer to the problem, according to Smallwood, lies in raising awareness. He reportedly continued: "We need to do all we can to raise awareness of the seriousness of diabetes and help people understand how a healthy lifestyle can help reduce their risk of developing type 2 diabetes."
Diabetes News Archive
http://www.diabetes.co.uk/news/index.html
Syringe installation to raise diabetes awareness - Mon, 11 May 2009
Walnuts and diabetes - Thu, 07 May 2009
New website for diabetes sufferers - Thu, 07 May 2009
Diabetes company to cut 200 jobs - Tue, 05 May 2009
Type 1 diabetes and sexual dysfunction - Tue, 05 May 2009
Diabetes drug could cause pancreas problems - Fri, 01 May 2009
DVLA facing petition about diabetes stance - Thu, 30 Apr 2009
Diabetes risk prevention could be harder for men - Thu, 30 Apr 2009
Diabetes causes greater risk of stroke - Tue, 28 Apr 2009
Diabetes drug fails in study - Mon, 27 Apr 2009
Making Third world diabetes drugs cheaper - Mon, 27 Apr 2009
New diabetes DVD for education - Fri, 24 Apr 2009
Many type 1 diabetes cases are misdiagnosed - Thu, 23 Apr 2009
Diabetes, gluten and schizophrenia linked - Wed, 22 Apr 2009
New stem cell treatment for diabetes could replace insulin - Mon, 20 Apr 2009
Diabetes UK to lead care training - Fri, 17 Apr 2009
Diabetes television study - Fri, 17 Apr 2009
Diabetes in Saudi Arabia - Thu, 16 Apr 2009
Stem cells to delay type 1 diabetes onset - Wed, 15 Apr 2009
Good fat can prevent diabetes - Tue, 14 Apr 2009
Diabetes epidemic in Scotland - Tue, 07 Apr 2009
Diabetes drug carries unknown tumour risk - Fri, 03 Apr 2009
Obese cows prone to developing diabetes - Fri, 03 Apr 2009
Journal retracts diabetes study - Thu, 02 Apr 2009
Diabetes drug found to be superior - Wed, 01 Apr 2009
Stress related to diabetes can influence blood glucose - Wed, 01 Apr 2009
NHS will suffer from Wales obesity, diabetes crisis - Mon, 30 Mar 2009
Care trusts failing to raise awareness of diabetes - Mon, 30 Mar 2009
Influence of fructose on diabetes - Fri, 27 Mar 2009
Diabetes drugs under review - Fri, 27 Mar 2009
Diabetes linked to Alzheimers - Thu, 26 Mar 2009
Sled dogs and diabetes - Wed, 25 Mar 2009
Diabetes UK campaign cleared by advertising authority - Wed, 25 Mar 2009
New calculator for diabetes risk - Tue, 24 Mar 2009
Diabetes results will be displayed differently - Mon, 23 Mar 2009
Diabetes drug grown in tobacco plants - Thu, 19 Mar 2009
Testosterone lower amongst men with type 2 diabetes - Mon, 16 Mar 2009
Chocolate tax to control obesity and diabetes - Fri, 13 Mar 2009
Sleep linked to diabetes - Thu, 12 Mar 2009
Diabetes drug link challenged - Wed, 11 Mar 2009
Spike in diabetes in Saudi Arabia - Tue, 10 Mar 2009
Change 4 life campaign with diabetes elements causes controversy - Tue, 10 Mar 2009
Medication given to diabetes patients too early - Mon, 09 Mar 2009
Diabetes and a genetic link - Fri, 06 Mar 2009
Virus that triggers child diabetes - Fri, 06 Mar 2009
Diabetes causing drug information buried - Mon, 02 Mar 2009
Diabetes could be tackled by surgery - Mon, 02 Mar 2009
Diabetes rates soar in the UK - Tue, 24 Feb 2009
Diabetes leap linked to unhealthy living - Tue, 24 Feb 2009
Diabetes cancer and heart charities unite - Mon, 23 Feb 2009
False diabetes treatments under investigation - Fri, 20 Feb 2009
Pedal power for diabetes cure - Fri, 20 Feb 2009
New online diabetes resource - Thu, 19 Feb 2009
Multimedia support for type 1 diabetes children - Thu, 19 Feb 2009
Type 1 diabetes treatment breakthrough - Wed, 18 Feb 2009
Charity warns of blindness risk - Wed, 18 Feb 2009
Diabetes drug losing momentum - Mon, 16 Feb 2009
Health PR firm will handle diabetes drug - Fri, 13 Feb 2009
Tattoos to control diabetes - Fri, 13 Feb 2009
New resource from diabetes charity - Thu, 12 Feb 2009
Further reports of health service diabetes failures - Thu, 12 Feb 2009
Diabetes most likely amongst south Asians - Wed, 11 Feb 2009
Psychological support from nurses could help diabetes patients - Wed, 11 Feb 2009
Energy drink causes diabetes in Ghana - Mon, 09 Feb 2009
Neuropathy healing from bone marrow cells - Fri, 06 Feb 2009
Diet low in GI better than high-fibre for people with diabetes - Thu, 05 Feb 2009
Celebrity loses pounds for Diabetes UK - Wed, 04 Feb 2009
NHS failing people with diabetes - Wed, 04 Feb 2009
Diabetes risk due to intake of eggs - Tue, 03 Feb 2009
Minority diabetes awareness drive - Tue, 03 Feb 2009
Obese and diabetics could be helped by gastric device - Mon, 02 Feb 2009
Pharmaceutical company will shed thousands of jobs - Mon, 02 Feb 2009
New sensor makes diabetes and exercise clearer - Fri, 30 Jan 2009
Diabetes company sees potential in Russia - Fri, 30 Jan 2009
Diabetes care amongst poorer countries - Thu, 29 Jan 2009
Life expectancy high alongside diabetes - Thu, 29 Jan 2009
Government health profile indicates increases in diabetes - Wed, 28 Jan 2009
Bursts of exercise lower diabetes risk - Wed, 28 Jan 2009
Exposure to chemicals may increase diabetes risk - Tue, 27 Jan 2009
Type 2 diabetes patients should get CBT from nurses and GPs - Tue, 27 Jan 2009
Weekly injection could aid type 2 diabetes treatment - Mon, 26 Jan 2009
Diabetes pill could see end of injections - Mon, 26 Jan 2009
Major diabetes risk amongst Maoris - Fri, 23 Jan 2009
Diabetes and psychological problems - Thu, 22 Jan 2009
6000 volunteers for diabetes study - Wed, 21 Jan 2009
NHS direct support people with diabetes - Wed, 21 Jan 2009
Diabetes pregnancy needs blood pressure control - Tue, 20 Jan 2009
First saliva test for type 2 diabetes - Tue, 20 Jan 2009
Laughter good for diabetes - Mon, 19 Jan 2009
Diabetes campaign causes bullying - Mon, 19 Jan 2009
New NHS budgets could benefit diabetes patients - Fri, 16 Jan 2009
Sleep-wake rhythm and diabetes - Fri, 16 Jan 2009
Chewing gum for diabetes aid - Thu, 15 Jan 2009
Diabetes program calls for healthy eating in Hispanic community - Thu, 15 Jan 2009
Diabetes in Wales increasing - Wed, 14 Jan 2009
Diabetes and obesity campaign draws fire - Wed, 14 Jan 2009
Vitamin D could prevent diabetes - Tue, 13 Jan 2009
Diabetes and brain injury link - Tue, 13 Jan 2009
Oats trial seeking people with diabetes - Mon, 12 Jan 2009
Diabetes screening plan causing concern in Ireland - Mon, 12 Jan 2009
Diabetes cases rising all the time - Fri, 09 Jan 2009
Great 2008 for American diabetes association - Fri, 09 Jan 2009
Gum disease treatment for diabetes patients - Thu, 08 Jan 2009
Alzheimers disease affected by diabetes - Thu, 08 Jan 2009
Northern Ireland needs a diabetes strategy - Wed, 07 Jan 2009
Similar mortality between diabetes and heart disease - Wed, 07 Jan 2009
Low-carb diabetes diets proving effective - Tue, 06 Jan 2009
One diabetes diagnosis every three minutes in UK - Tue, 06 Jan 2009
Diabetes protection from larger bottom - Mon, 05 Jan 2009
Mental slowdown possible for people with diabetes - Mon, 05 Jan 2009
Gestational diabetes risk higher amongst some women - Fri, 02 Jan 2009
Diabetes and blood sugar levels affect memory - Wed, 31 Dec 2008
Diabetes and celiac shares genetic origin - Tue, 30 Dec 2008
Parental influence on diabetes - Tue, 30 Dec 2008
Surgery reverses diabetes in teens - Mon, 29 Dec 2008
Vitamin reverses kidney disease amongst diabetics - Mon, 29 Dec 2008
Type 1 diabetes could be triggered by child virus - Wed, 24 Dec 2008
Eight month delay to diabetes drug - Wed, 24 Dec 2008
Christmas over eating could put thousands at diabetes risk - Tue, 23 Dec 2008
Diabetes drug agreement signed - Tue, 23 Dec 2008
Vitamin D supplements reduce the risk of Type 1 diabetes - Wed, 17 Dec 2008
New evidence suggests links between Diabetes and Lymphoma - Tue, 16 Dec 2008
Increased risk of diabetes if you eat an egg everyday - Mon, 15 Dec 2008
Type 1 diabetes and coeliac disease share genetic origin - Thu, 11 Dec 2008
Increased bone risk due to diabetes drugs - Wed, 10 Dec 2008
New ExtendBar could help diabetics control blood sugar levels - Tue, 09 Dec 2008
Poor sleepers face greater diabetes risk - Tue, 09 Dec 2008
Lower income children more affected by diabetes - Mon, 08 Dec 2008
Diabetes clue from body clock - Mon, 08 Dec 2008
Diabetes drugmaker gives optimistic forecast - Fri, 05 Dec 2008
New advanced diabetes centre - Fri, 05 Dec 2008
Vege food could lower cholesterol and reduce diabetes risk - Thu, 04 Dec 2008
Diabetes drug will include warning - Thu, 04 Dec 2008
Coffee lowers risk of diabetes - Wed, 03 Dec 2008
Diabetes time bomb in the Asian community - Wed, 03 Dec 2008
Company files for diabetes drug application - Tue, 02 Dec 2008
Risk of passing diabetes in pregnancy - Tue, 02 Dec 2008
Diabetes spending could soar in Australia - Mon, 01 Dec 2008
Call for diabetics to help each other - Mon, 01 Dec 2008
Diabetes cure from gastric surgery - Fri, 28 Nov 2008
Diabetes and obesity will cut life span - Thu, 27 Nov 2008
Life saving diabetes hospital team - Thu, 27 Nov 2008
Losing potassium could provoke diabetes - Wed, 26 Nov 2008
Heart risk genes exacerbated in diabetics - Wed, 26 Nov 2008
Using the internet to fight diabetes - Tue, 25 Nov 2008
Avandia risk higher than other diabetes drugs - Tue, 25 Nov 2008
Diabetes control through psychotherapy - Mon, 24 Nov 2008
Garlic based diabetes tablets - Mon, 24 Nov 2008
Avoid eggs, people with diabetes warned - Fri, 21 Nov 2008
Diabetes care in Norfolk concerning - Fri, 21 Nov 2008
New mobile phone diary for diabetes healing - Thu, 20 Nov 2008
GPS will begin widespread pre-diabetes screening - Wed, 19 Nov 2008
Diabetes risk increased by HIV medicines - Tue, 18 Nov 2008
Leukaemia drug could prove effective for diabetes - Tue, 18 Nov 2008
Diabetes day highlighted by building - Mon, 17 Nov 2008
Children with diabetes lobby parliament - Mon, 17 Nov 2008
American Diabetes Month of November - Wed, 12 Nov 2008
Question over diabetes and aspirin - Wed, 12 Nov 2008
Large Pfizer donation to fight diabetes - Tue, 11 Nov 2008
Diabetes survey for children launched - Tue, 11 Nov 2008
Breakthroughs in diabetes treatment - Mon, 10 Nov 2008
Gestational diabetes could affect child language - Mon, 10 Nov 2008
Pre-diabetes still unknown - Fri, 07 Nov 2008
Diabetes epidemic could be prevented - Fri, 07 Nov 2008
TV show pulled over diabetes row - Thu, 06 Nov 2008
Florida has booming diabetes population - Thu, 06 Nov 2008
Type 1 diabetes this November - Wed, 05 Nov 2008
Red wine drug could help fight diabetes - Wed, 05 Nov 2008
Twice weekly fish could help diabetes patients - Tue, 04 Nov 2008
Higher diabetes drug use amongst young - Tue, 04 Nov 2008
Further calls to ban diabetes drug - Mon, 03 Nov 2008
Company sponsors diabetes day - Mon, 03 Nov 2008
Group calls for ban of diabetes drug - Fri, 31 Oct 2008
Diabetes doubles in ten years - Fri, 31 Oct 2008
Type 1 diabetes and the artificial pancreas - Thu, 30 Oct 2008
New spice for diabetes - Thu, 30 Oct 2008
Open diabetes day to raise awareness - Mon, 27 Oct 2008
Life expectancy fall caused by diabetes - Mon, 27 Oct 2008
Diabetes treatment cost impacts on NHS - Fri, 24 Oct 2008
Diabetes UK in Second Life - Fri, 24 Oct 2008
New Welsh guidelines for diabetes management - Thu, 23 Oct 2008
Diabetes drugmaker looking to stem cells - Thu, 23 Oct 2008
Diabetes complication linked with heart attacks - Wed, 22 Oct 2008
Diabetes drug supply deal - Wed, 22 Oct 2008
New company in type 2 diabetes development - Tue, 21 Oct 2008
Diabetes cell transplant approved in New Zealand - Tue, 21 Oct 2008
200,000 Scots suffering from diabetes - Mon, 20 Oct 2008
2.5 million people with diabetes in the UK - Mon, 20 Oct 2008
Aspirin use for diabetes patients under question - Fri, 17 Oct 2008
Diabetes not a Parkinson's disease risk - Fri, 17 Oct 2008
Diabetes test patent given to company - Thu, 16 Oct 2008
Imperial college say 10,000 will walk for diabetes - Thu, 16 Oct 2008
Scottish GPs have wider diabetes treatment options - Wed, 15 Oct 2008
Type 2 diabetes linked to tuberculosis - Wed, 15 Oct 2008
Diabetes breath test in development - Tue, 14 Oct 2008
Diabetes drug treatment hope - Tue, 14 Oct 2008
Bradford diabetes inquiry - Mon, 13 Oct 2008
Coffee and diabetes control - Mon, 13 Oct 2008
Tai chi and diabetes - Fri, 10 Oct 2008
Diabetes risk increased by antidepressant drugs - Fri, 10 Oct 2008
Diabetes cure closer due to Edinburgh stem cell breakthrough - Thu, 09 Oct 2008
Novel diabetes drug could be effective - Thu, 09 Oct 2008
Northern Ireland totals diabetes cost of GBP1 million day - Wed, 08 Oct 2008
Cost of diabetes hits GBP1 million per hour - Wed, 08 Oct 2008
ResMed call for links between diabetes and apnoea to be recognised - Tue, 07 Oct 2008
Massive NHS obesity and diabetes bill - Tue, 07 Oct 2008
Diabetes Walk a great success - Mon, 06 Oct 2008
Diabetes UK launch new campaign - Mon, 06 Oct 2008
New type 1 diabetes website and magazine for children - Thu, 02 Oct 2008
UK gets second for diabetes care - Thu, 02 Oct 2008
Award for innovator featured by Abbott Diabetes Care - Wed, 01 Oct 2008
EndoBarrier a diabetes treatment potential - Wed, 01 Oct 2008
Diabetes awareness campaign launched by IDF - Tue, 30 Sep 2008
Ireland ninth for diabetes care - Tue, 30 Sep 2008
NHS diabetes care still not diagnosing accurately - Mon, 29 Sep 2008
New diabetes retinopathy drug research - Mon, 29 Sep 2008
New diabetes drug target - Fri, 26 Sep 2008
Positive diabetes drug data revealed - Fri, 26 Sep 2008
Fresh diabetes drug found to work - Thu, 25 Sep 2008
Diabetes rise must be stemmed, experts say - Thu, 25 Sep 2008
Diabetes patients find limited use in online records - Wed, 24 Sep 2008
Diabetes drug company call for approval - Wed, 24 Sep 2008
Female diabetes and low bone density - Tue, 23 Sep 2008
Nasal insulin not effective for type 1 diabetes - Tue, 23 Sep 2008
Study to assess drugs in adolescents with diabetes - Mon, 22 Sep 2008
New diabetes treatment hope - Mon, 22 Sep 2008
Lack of sunshine in Scotland could up diabetes risk - Thu, 18 Sep 2008
Diabetes UK release new viral film - Thu, 18 Sep 2008
Cutting diabetes risk through exercise - Wed, 17 Sep 2008
Chemical linked with diabetes - Wed, 17 Sep 2008
Lupins could hold diabetes cure - Tue, 16 Sep 2008
Men need to work harder to beat diabetes - Tue, 16 Sep 2008
Diabetes blindness risk reduced with ARBs - Mon, 15 Sep 2008
Chamomile tea helps diabetes - Mon, 15 Sep 2008
Diabetes prevention using dance - Fri, 12 Sep 2008
New Latino toolkit from American Diabetes Association - Fri, 12 Sep 2008
Early blood glucose control in diabetes positive - Thu, 11 Sep 2008
Diabetes drug conclusion announced - Thu, 11 Sep 2008
Diabetes treatment protects the kidneys - Wed, 10 Sep 2008
Diabetes drug company trial hitch - Tue, 09 Sep 2008
Better diabetes control with continuous devices - Tue, 09 Sep 2008
Treatment hope for diabetes sufferers - Mon, 08 Sep 2008
NHS failure to diagnose diabetes - Mon, 08 Sep 2008
Diabetes prevention and care in UK progressing - Fri, 05 Sep 2008
Gastic bypass quickly reverses diabetes symptoms - Thu, 04 Sep 2008
Scientists change mouse cells to treat diabetes - Thu, 04 Sep 2008
Tata to shift focus to diabetes - Tue, 02 Sep 2008
Vitamin D to protect against diabetes - Tue, 02 Sep 2008
Child diabetes treatment expansion - Mon, 01 Sep 2008
Swimming for diabetes - Mon, 01 Sep 2008
Diabetes drug class carries risk - Fri, 29 Aug 2008
Sick fat cells could cause type diabetes - Fri, 29 Aug 2008
More technology in diabetes care - Thu, 28 Aug 2008
Healthcare for people with diabetes variable - Thu, 28 Aug 2008
Further deaths due to diabetes drug - Wed, 27 Aug 2008
Cholesterol, cancer and diabetes associations - Wed, 27 Aug 2008
Diabetes bread remedy - Tue, 26 Aug 2008
Diabetes risk for caesarean deliveries - Tue, 26 Aug 2008
Diabetes linked to sugary drinks - Fri, 22 Aug 2008
Diabetes and obesity epidemic in Australia - Fri, 22 Aug 2008
Government slammed over diabetes reports - Thu, 21 Aug 2008
Diabetes linked with arsenic in water - Thu, 21 Aug 2008
Byetta diabetes drug subject to warnings - Tue, 19 Aug 2008
Diabetics should have pneumonia vaccination - Tue, 19 Aug 2008
Cystic fibrosis and diabetes linked - Mon, 18 Aug 2008
New potential blockbuster diabetes drug - Mon, 18 Aug 2008
Diabetes research initiative announced - Fri, 15 Aug 2008
Diabetes and school - Fri, 15 Aug 2008
Diabetes pilot recruitment underway - Thu, 14 Aug 2008
Baked Sweet Potato Fries
This simple recipe stars sweet potatoes which are
high in fiber, beta carotene, and potassium.
Makes 4 Servings
Ingredients:
-
2 pounds sweet potatoes
(approximately 2 large) -
Salt & pepper to taste
-
1 Tablespoon olive
Directions:
Preheat oven to 450 degrees.
Scrub and rinse sweet potatoes, pat dry. Leaving skin on, cut the sweet potatoes into thick strips (resembling french fries).
In a bowl, gently toss the sweet potatoes with oil to coat. Place on a baking sheet in a single layer. Sprinkle with salt and pepper if desired.
Bake 10 minutes, gently turn the sweet potatoes over to brown the other side and bake 10 minutes more, or until lightly browned.
Quinoa is a grain that is a good source of protein, calcium, and iron. It can be found in most health food stores.
1) Prepare the quinoa
- 1 cup quinoa
- 2 cups water
Rinse quinoa in cool water. Bring 2 cups water to a boil. Add quinoa and simmer for 15 min.
2) Prepare the asparagus
- 1 pound fresh asparagus - wash; slice diagonally into 2 inch pieces
- 2 teaspoons olive oil
- salt and pepper to taste
Heat oil in a medium frying pan. Add asparagus and salt and pepper. Stir constantly until asparagus is tender but still somewhat crisp (approximately 5 minutes)
3) Combine quinoa and asparagus or serve separately if desired. Enjoy!
Makes 4 servings.
Per serving:
- 200 calories
- 35 g carbohydrate
- 5.5 g fiber
- 24 g protein
- 4 g fat
Spinach Artichoke Dip
-
5 ounces fresh spinach, rinsed and stemmed
-
2 garlic cloves, pressed or minced
-
1 1/2 cups cooked butter beans or cannellini (15-ounce can, drained and rinsed)
-
1 cup chopped scallions
-
2 tablespoons chopped fresh basil
-
2 to 3 tablespoons fresh lemon juice, to taste
-
5 to 6 artichoke hearts or bottoms, minced (15-ounce can)
-
salt and ground black pepper to taste
Steam the spinach until just wilted (2-3 minutes). Drain.
In a food processor or blender, puree the spinach, garlic, beans, scallions, basil and 2 tablespoons of the lemon juice until very smooth. Fold in the minced artichoke hearts and add more lemon juice and salt and pepper to taste. Serve chilled or at room temperature.
Makes 3 cups
Per 3 tablespoon serving:
-
26 calories
-
1 g fat
-
5.3 g carbohydrate
-
2.3 g fiber
-
1.8 g protein
Tofu Brochettes
From “Food for Life - How the New Four Food Groups Can Save Your Life” by Dr. Neal Barnard, M.D.
These are perfect for a barbecue or summer outing. Grill them and serve with cooked brown rice or bulgur.
Ingredients:
-
1 pound firm tofu
-
2 teaspoons dried oregano
-
1 cup water
-
1/2 cup soy sauce
-
1/2 cup balsamic vinegar or wine vinegar
-
1/2 cup red wine (optional)
-
1/4 teaspoon black pepper
-
Suggested vegetables:
-
Red onion
-
Green bell pepper
-
Red bell pepper
-
Button mushrooms
-
Japanese eggplant
-
Zucchini
-
Cherry tomatoes
-
Press the tofu to remove some of its moisture: Place on a cutting board or baking sheet and cover with a second cutting board or baking sheet. Put 2 or 3 heavy items (like cans of beans) on top of this and let it stand at least 30 minutes.
In the meantime, toast the oregano in a large, dry skillet over medium-low heat for 2 to 3 minutes. Add the remaining marinade ingredients and stir to mix. Remove from heat. Cut the pressed tofu into 1-inch cubes and add to the marinade. Allow the tofu to marinate for at least 1 hour, occasionally turning it gently.
Cut the onion into 1-inch chunks. Seed the peppers and cut them into large pieces. Clean the mushrooms. Slice the eggplant and zucchini into 1/2-inch-long pieces.
Place an assortment of vegetables and marinated tofu onto each skewer, and grill under a broiler or over coals, turning every few minutes to expose all sides to the heat. Cook 5 to 10 minutes, until vegetables are lightly browned and everything is hot.
Makes 6-8 servings
Per 1/8 recipe (not including rice or bulgur)
-
Calories 45
-
Carbohydrates 5
-
Protein 3.5
-
Fiber 1
-
Fat
Portabello mushrooms in this dish have a meaty texture and flavor and take the place of the usual beef or chicken found in fajitas.
Fajita filling:
Slice the following into long, thin strips:
- 4 large Portabello mushroom caps
- 2 large onions
- 2 large green peppers
- 1 large red pepper
Combine in a shallow dish:
- 2 Tbsp white wine vinegar
- 2 tsp vegetable oil
- 2 Tbsp finely minced cilantro
- 1 Tbsp finely minced garlic
- 1 tsp ground cumin
- 1/2 tsp paprika
- 1/4 tsp black pepper
- 1/2 tsp salt
- 1 tsp chili powder
Add sliced vegetables to vinegar mixture and marinate for 15 - 30 minutes.
Place vegetables in a large nonstick skillet over medium-high heat for 5 minutes or until vegetables are cooked but still slightly crisp. Drain any left-over liquid and place vegetables in a serving dish.
Roll vegetables inside a 6-inch whole wheat tortilla.
Add your choice of toppings:
- reduced fat cheddar cheese
- salsa
- low fat sour cream or plain yogurt
- mashed avocado
Makes 6 fajitas
Per fajita (not including toppings):
- 225 calories
- 8 g protein
- 8 g fat
- 30 g carbohydrate
Very Veggie Slaw
A quick and easy way to throw together a colorful, tasty salad full of healthy vitamins and antioxidants!
- 1 cup shredded broccoli stalks
- 1 cup shredded white cabbage
- 1 cup shredded red cabbage
- 1 cup shredded carrot
In a large bowl, combine all vegetables and toss.
- 1 tablespoon lemon juice
- 2 tablespoons sweet relish
- 1/2 teaspoon salt
- 1/4 teaspoon dill
- 1/4 teaspoon pepper
- 1/4 teaspoon celery seed
- 1/4 teaspoon dry mustard
- 3/4 cup fat free or low fat mayonnaise
In a small bowl, combine all above ingredients. Toss with vegetables in the large bowl.Chill well.
Makes 4 servings
Per serving:
- 75 calories
- 4 g protein
- 3 g fat
- 3 g fiber
- 5 g carbohydrate
Summer Zucchini Bread Beat together egg whites, oil, zucchini, and apple juice concentrate. Mix together flour, cinnamon, and baking soda. Add flour mixture to zucchini mixture and stir until just moistened. Pour batter into two non-stick 9x5x2 3/4 inch loaf pans. Bake 35 minutes or until knife inserted into the loaves comes out clean. Makes 14 servings (7 per loaf)
Per serving:
Black and Red Bean Salad with Lime-Cumin Dressing
Recipe by Cyndi Reeser
The dressing makes this high fiber salad special. So quick and easy, especially if you keep a supply of the salad dressing on hand. Then you can combine the dressing with any combination of beans you like!
Salad:
- 1 cup thinly sliced celery (2 stalks)
- 3/4 cup vertically sliced red onion
- 1 (15 oz.) can of black beans
- 1 (15 oz.) can of dark red kidney beans
Dressing:
- 1/2 cup fresh lime juice
- 2 Tbsp. sugar
- 2 Tbsp. olive oil
- 1/2 tsp. ground cumin
Instructions:
Rinse and drain the canned beans. Combine with the celery and onion in a large bowl and toss well. In a separate bowl, combine ingredients for the dressing and stir with a whisk until blended. Pour half of the dressing over the bean mixture, tossing to coat. Adjust seasonings as desired. Refrigerate the remainder of the dressing in a jar for your next bean salad!
Makes 4 - one cup servings
Per 1 cup serving:
- calories 245
- carbohydrate 41 g
- protein 13 g
- fiber 7 g
- fat 4.5 g
Quinoa Salsa Salad This nutritious and easy to make salad is delicious as a side dish or main course! Combine together in a mixing bowl: Cover and let chill in the refrigerator for at least one hour. *If you can't find quinoa, substitute whole grain couscous or rice instead. Makes 4 Servings
Per Serving:
Salmon-Rice Salad with Dilled Cucumber Dressing Stay cool as a cucumber with this refreshing and oh so easy main course salad! Ingredients: Prepare Dilled Cucumber Dressing. Arrange cucumber slices, overlapping edges, in circle on each of 4 plates. Toss together salmon, wild rice, white rice, green onions, and cherry tomatoes; spoon into center of cucumbers. Spoon Dilled Cucumber Dressing over salads. Cover and refrigerate until chilled. Dilled Cucumber Dressing: Place all ingredients in blender. Cover and blend at high speed until smooth (about 15 seconds). Makes 4 servings
Per serving:
Spinach Bean Soup
Warm up with this healthy and easy to cook soup. The beans are high in fiber to satisfy your hunger and the spinach adds a healthy dose of vitamin A.
Makes 6 Servings
Ingredients:
- 1 cup chopped onions
- Choice of either: 1/2 cup chopped celery or mushrooms
- 1 Tbsp. canola oil
- 1 - 10 oz. package frozen chopped spinach
- 2 16 oz cans Cannellini beans (white kidney beans), drained and rinsed
- 1 quart of Vegetable broth or fat free chicken broth
- 1/2 tsp. salt
- 1/4 tsp. dried thyme
- Optional: other seasonings as desired
Directions:
In a large heavy pot, simmer the onions and celery in the oil until soft, over medium heat.
Add all remaining ingredients.
Cover and cook on low heat for 15 or 20 minutes, stirring occasionally
Adjust seasonings to your taste and serve.
Cannellini Bean Paté Appetizer
Recipe by Cyndi Reeser, MPH, RD, LD
This bean paté(paste) is fat-free and an excellent source of protein and iron. It can be made of just about any type of bean; however, the cannellini bean (white kidney bean) mashes up easily by hand and has a particularly suitable moisture and texture for this dish. Use it as a sandwich spread or as a dunk for assorted raw vegetables and crackers.
Ingredients:
-
1 pound can of white kidney beans
-
1Tbsp. finely chopped celery
-
1 Tbsp. finely chopped sweet red pepper
-
1 Tbsp. finely chopped fresh parsley or cilantro
-
1 tsp. lemon juice or vinegar
-
1/4 tsp. onion powder
-
1/4 tsp. garlic powder
-
1/2 tsp. cumin
-
1 tsp. salt
Directions:
Rinse and drain the canned beans and place them in a mixing bowl.
Mash the beans with a potato masher until uniformly smooth
Stir in all the remaining ingredients and blend well.
Adjust the seasonings to suit your taste. Transfer to a storage container or serve right away with assorted raw vegetables, whole grain bread, or crackers.
Sweet Potato with Cranberries
Ingredients:
-
4 medium sized sweet potatoes, peeled and cut into chunks
-
1 large Granny Smith apple, peeled and diced
-
1 cup raw cranberries, washed
-
1/2 cup orange juice
Directions:
Combine all ingredients in a large casserole dish.
Cover and bake for 1 hour and 15 minutes, or until tender.
Makes 8 servings
Per serving:
-
90 calories
-
20 g carbohydrate
-
3 g fiber
-
0 g fat
-
1 g protein
Harvest Vegetable Corn Muffins
Use squash, pumpkin, or sweet potato to make these muffins both moist and lower in fat.
Ingredients:
-
1 cup whole wheat flour
-
1 cup cornmeal
-
4 tsp. baking powder
-
1/4 cup sugar
-
1/2 tsp. salt
-
1 egg
-
1/2 cup milk or soymilk
-
2 Tbsp. canola oil
-
1/2 cup of one of the following fresh, frozen, or canned vegetables that has been cooked and mashed: butternut squash, sweet potato, or pumpkin.
Directions:
Preheat oven to 400 degrees.
Grease 12 cup muffin tin with non-stick cooking spray.
Mix together dry ingredients in a medium bowl.
Mix together wet ingredients in a small bowl. Add to the dry mixture and stir until just blended.
Pour mixture into muffin tin, filling cups 3/4 full.
Bake for 20 to 25 minutes.
Blueberry Crisp Filling: Toss together flour and sugar. Mix together with blueberries and place in a 9x9 inch glass baking dish. Topping: Mix all topping ingredients together. Sprinkle on top of blueberry filling. Bake at 350 degrees for 45 minutes. Makes 6 servings. Per Serving:
Chocolate Nut Balls
The nuts and dark chocolate add healthy antioxidants to this yummy treat.
Ingredients:
- 2 ounces unsweetened (preferably dark)baking chocolate
-
2 Tablespoons vegetable oil
-
1/2 cup plus 2 tablespoons of water
-
1 cup date sugar
-
1 1/2 cup chopped almonds, pecans, or walnuts
Directions:
In a small saucepan, melt chocolate, oil and water over medium heat.
Reduce heat to low, add date sugar. Cook for 3 minutes, stirring constantly.
Remove pan from heat and stir in chopped nuts.
Drop by the spoonful and roll into 24 balls on a dish. If desired, roll in additional chopped nuts. Let balls cool. Store in the refrigerator or freezer.
Makes 24 balls
Per ball:
-
100 calories
-
1 g protein
-
8 g fat
-
7 g carbohydrate
Dark Chocolate Covered Strawberries A scrumptious dessert! Use dark chocolate instead of milk chocolate to reduce the amount of sugar in the recipe and gain many health benefits. Ingredients: Directions: Melt chocolate in a double boiler over low heat. (if you don't have a double boiler, a crock pot works well). Hold strawberries by the stem and dip them into the chocolate. Place on wax paper to cool. Refrigerate until ready to serve. Makes approximately 12 strawberries (depending on size of berries) * note - These dietary values assume that all 8 ounces of chocolate are used. The values will be less if you coat each strawberry with less chocolate. To further reduce the amount of carbohydrate, buy dark chocolate with as little sugar as possible.
Per 1/12 of the recipe*:
Oatmeal Flax Chocolate Chip Cookies
This recipe uses less sugar and replaces white flour with whole wheat flour and ground flaxseed to increase the fiber content. Flaxseed is also a good source of Omega-3 fatty acids. The coconut oil adds a nice flavor and is an excellent source of mid-chain fatty acids and one of the richest natural sources of lauric acid, which helps protect against infectious illnesses. (Of course, these are still cookies so eat in moderation as a treat.) Preheat oven to 375 degrees. Beat butter and coconut oil together with an electric mixer in a large bowl until light and fluffy. Add brown sugar and beat well. Add egg and vanilla and mix thoroughly. In a medium bowl, combine flour, flaxseed, baking soda, and salt. Gradually add flour mixture, then stir in oats and chocolate chips. Drop a heaping teaspoon of dough onto cookie sheets, leaving about 2 inches between each cookie. Bake 10 minutes or until lightly browned. Makes 4 dozen cookies
Per cookie:
This very simple recipe makes a refreshing and satisfying summertime dessert.
Ingredients:
- 3/4 cup ice
- 1/2 cup unsweetened strawberries (frozen and slightly thawed)
- 1/4 cup milk (or soy/rice milk)
- 1/4 cup vanilla frozen yogurt (or soy/rice frozen dessert)
- 1/8 teaspoon almond extract
Directions:
Combine ice, strawberries, and milk in a blender. Blend at high speed until ice is well crushed. Add frozen yogurt and almond extract and blend just until smooth.
Makes 1 serving
Per serving:
-
120 calories
-
21 g carbohydrate
-
4.5 g protein (depending on type of milk and frozen dessert used)
-
3 g fiber
Roasted Pumpkin Seeds
This crunchy snack is so easy and delicious there's no need to only make them at Halloween! Pumpkin seeds are a great source of magnesium, iron, zinc, essential fatty acids, and protein. They are also low in carbohydrate.
- 2 cups whole raw pumpkin seeds
- 1 tablespoon melted butter or oil
- salt to taste
Scrape seeds from the inside of a pumpkin. Rinse the pumpkin pulp off as well as you can and pat dry.
Preheat oven to 150 degrees F (75 degrees C). Roasting on this lower heat helps to maintain more of the healthy essential fatty acids.
Combine all ingredients in bowl; stir to coat all the seeds.
Spread the seeds in a single layer on a baking sheet. Bake until seeds are golden brown (about 20 minutes), stirring occasionally.
Adjust seasonings to suit your taste. Experiment: try adding a bit of brown sugar for sweet and salty seeds or paprika and celery salt for a spicy batch.
Makes 4 servings
Per 1/4 cup serving:
-
186 calories
-
6 g carbohydrate
-
1.5 g fiber
-
15 g fat
-
8 g protein